
When a patient walks into a hospital needing a life-saving drug and it’s not there, the consequences aren’t theoretical-they’re immediate. A child with leukemia waits 10 days for asparaginase. A cancer patient gets a less effective substitute that causes worse side effects. A heart surgery patient gets a different anticoagulant that adds 22% more time to their procedure. These aren’t rare exceptions. They’re happening every day across the U.S. because of drug shortages.
What’s Really Behind the Missing Medications?
Drug shortages aren’t random glitches. They’re the result of a broken system. About 83% of the drugs in short supply are generics-cheap, older medications that manufacturers barely make a profit on. When the price is low and the risk of a manufacturing error is high, companies walk away. The FDA found that 47% of shortages come from fractured global supply chains, especially when raw materials like active pharmaceutical ingredients come from just one country. Another 32% are caused by manufacturing quality issues-contaminated batches, failed inspections, or plants shut down for repairs. And 21%? Simply because the raw materials aren’t available. It’s not a matter of not making enough. It’s that no one wants to make the low-margin drugs that hospitals rely on every day. Heparin, IV saline, chemotherapy agents, antibiotics-these aren’t luxury items. They’re the backbone of modern medicine. But when a company can make more money producing a new $10,000 cancer drug than a $0.50 antibiotic, the math doesn’t add up for production.How Shortages Hurt Patients Directly
Patients don’t just get told, “We’re out.” They get alternatives. Sometimes those alternatives work. Often, they don’t. In oncology, shortages of drugs like nelarabine and asparaginase have forced delays of 7 to 14 days in treatment for children with acute lymphoblastic leukemia. That’s not just inconvenient-it’s dangerous. Every day without the right drug increases the risk of relapse. In one study, 42% of oncology shortages led to treatment changes that were less effective or more toxic. For patients with chronic pain, shortages of oral opioids mean they can’t refill prescriptions. Some skip doses. Others stop taking them entirely. A 2024 JAMA Network Open analysis found that nearly one in four patients facing a shortage either skipped doses, used less than prescribed, or didn’t fill the prescription at all. Even common drugs like lorazepam injection or triamcinolone are in short supply. That means ERs can’t sedate agitated patients. Diabetics can’t get insulin for emergencies. Patients with severe allergies can’t get epinephrine when they need it most. The NIH reports that 31% of hospitals have seen adverse events directly linked to drug shortages-things like allergic reactions from untested substitutes, overdoses from incorrect dosing, or infections from delayed antibiotics.
The Hidden Costs: Time, Labor, and Errors
Behind every missing drug is a team of pharmacists scrambling to fix it. Hospitals now spend an average of 15 to 20 hours per week per shortage just managing it. That’s not just calling suppliers. It’s reviewing alternatives, rewriting protocols, training staff, updating electronic systems, and documenting every change. Pediatric hospitals need even more time-25% more-because kids need special formulations that aren’t always available. When a hospital switches from one drug to another, mistakes spike. The NIH found that medication errors linked to shortages jumped from 38% in 2019 to 43% in 2024. Why? Because nurses aren’t trained on the new drug. Pharmacists are rushing. Dosing charts are outdated. A patient gets the wrong dose because the new drug looks different. A doctor prescribes a substitute they’re not familiar with. One hospital in Texas reported that switching from a shortage of IV heparin to an alternative anticoagulant added 22% more time to every cardiac procedure. Staff had to learn new monitoring rules, adjust infusion pumps, and double-check lab results. That meant fewer procedures per day. Longer wait times. More cancellations.Who’s Getting Left Behind?
It’s not just about what’s missing-it’s about who suffers most. Children, elderly patients, and those with chronic illnesses are hit hardest. A child with cancer can’t wait for a drug to come back. An elderly patient with heart failure can’t afford to miss a dose of diuretics. People on Medicaid or Medicare often can’t afford the more expensive alternatives. The American Hospital Association found that nearly 30% of Americans have skipped or cut back on medication because of cost-and drug shortages make that worse. When a $10 drug becomes a $100 substitute, patients choose between food and medicine. The AHA estimates that 1.1 million Medicare patients could die over the next decade because they can’t afford their prescriptions. Outpatient infusion centers are especially vulnerable. Forty-one percent of patients there have had treatments delayed, skipped, or canceled due to shortages. That means cancer patients miss weeks of therapy. Rheumatoid arthritis patients go without their biologics. Migraine sufferers lose access to their only effective relief.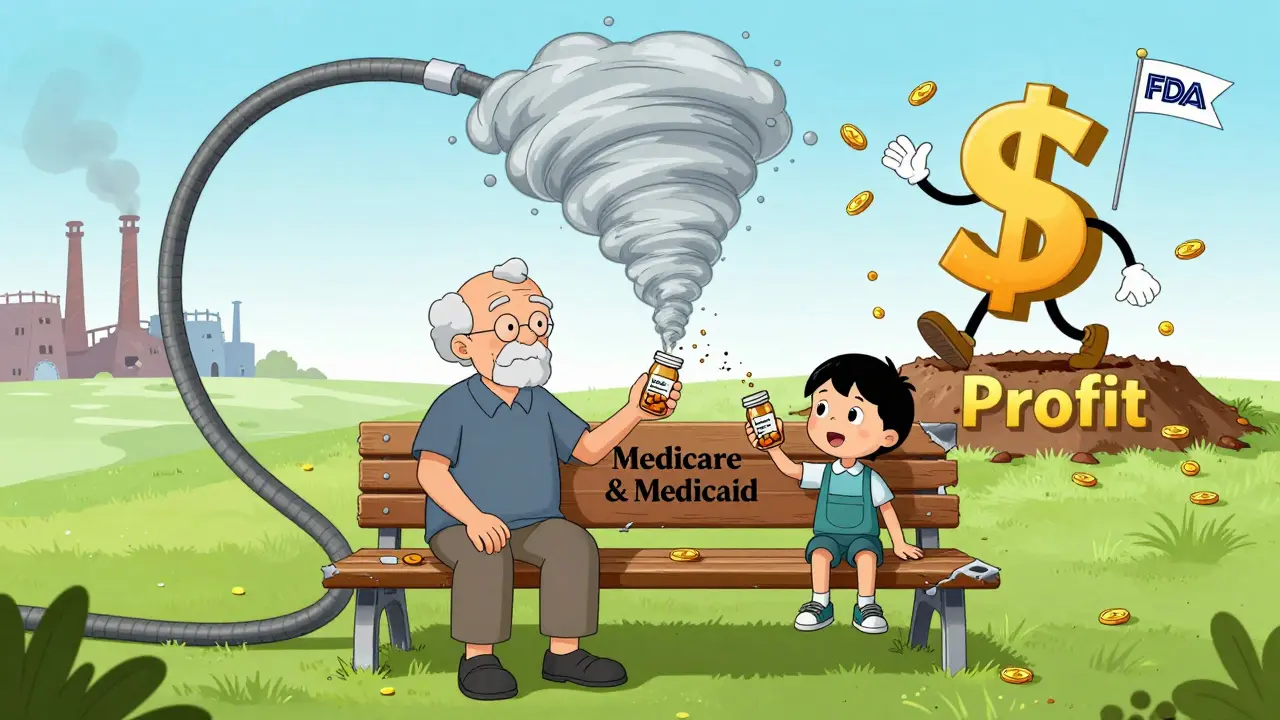
What’s Being Done-and Why It’s Not Enough
There are efforts to fix this. The FDA now requires manufacturers to report potential shortages six months in advance. That sounds good-until you realize most shortages happen with no warning at all. Companies still delay reporting because they fear losing business or triggering panic. Group purchasing organizations like Vizient have helped hospitals avoid $300 million in inventory costs since 2023 by pooling demand and sharing alerts. But that doesn’t solve the root problem: no one wants to make the cheap drugs. Some hospitals are building shortage management teams, investing in real-time tracking software, and stockpiling critical medications. But that’s expensive. Smaller clinics and rural hospitals can’t afford it. The government has held hearings. Congress has introduced bills. But no one has tackled the core issue: the economic model that makes producing generic drugs unprofitable. Until manufacturers are incentivized to make these essential, low-margin drugs-through guaranteed contracts, tax breaks, or price floors-shortages will keep coming.What This Means for You
If you or someone you love depends on a regular medication, don’t assume it’ll always be available. Talk to your pharmacist. Ask: “Is this drug in short supply? Are there alternatives? What happens if we run out?” Keep a 14-day supply on hand if possible. Don’t wait until the last refill. If your prescription is suddenly changed without explanation, ask why. Is it because of a shortage? Is the new drug safer? More effective? Or just cheaper for the pharmacy? And if you’re a caregiver, advocate. Share your story. Contact your representative. Drug shortages aren’t an abstract policy issue-they’re a daily threat to real people. The system is broken. And until it’s fixed, patients will keep paying the price.Comments (10)
-
Sarah Little January 4, 2026
The structural inefficiencies in the generic pharma supply chain are a classic case of market failure. The FDA’s current reporting mandates are reactive, not predictive, and the lack of price floors disincentivizes production of essential low-margin agents. We’re essentially outsourcing critical infrastructure to jurisdictions with volatile regulatory environments-India and China-without contingency planning. The result? Systemic fragility.
-
innocent massawe January 6, 2026
😢 This hits hard. In Nigeria, we don’t even have the luxury of shortages-we just don’t get the drugs at all. If a child needs asparaginase and it’s not here, there’s no backup. No hospital team. No tracking software. Just silence. The world talks about ‘shortages’ like it’s a glitch. For us, it’s a death sentence.
-
Tru Vista January 6, 2026
OMG. So like, the FDA says ‘report 6 months ahead’ but companies don’t? LMAO. Ofc they don’t. Why would they? They’re not gonna lose money on $0.50 drugs. And now nurses are giving wrong doses bc they’re tired and confused. This is a disaster. #healthcareisbroken
-
Angela Fisher January 6, 2026
They’re doing this on purpose. The Big Pharma lobby is pushing new drugs-$10k/month cancer drugs-so they can make billions. Meanwhile, the cheap stuff? Let it vanish. Then they sell you the ‘alternative’ at 20x the price. The government knows. The FDA knows. They’re letting this happen so you’ll pay more. It’s not a shortage. It’s a scheme. 🤫💸
-
Neela Sharma January 7, 2026
When the medicine vanishes so does the dignity of care
Children wait. Elders tremble. Nurses cry in the supply closet
We treat drugs like commodities when they are lifelines
Profit margins don’t heal broken bones or stop seizures
What if your mother’s insulin was a gamble?
What if your child’s chemo was a waiting game?
Then you’d know this isn’t policy
This is cruelty dressed as economics
-
Shruti Badhwar January 8, 2026
While the systemic issues are undeniable, it is imperative to acknowledge that regulatory harmonization across international manufacturing hubs could mitigate supply chain vulnerabilities. Furthermore, public-private partnerships aimed at securing raw material procurement may offer a viable pathway toward stabilization of generic drug availability.
-
Michael Burgess January 8, 2026
My cousin’s a nurse in rural Ohio. She told me last week they ran out of epinephrine for two days. Two. Days. A kid came in with anaphylaxis. They had to use an expired EpiPen they found in the back. It worked. But what if it hadn’t? We’re not talking about ‘inefficiencies’ here. We’re talking about people surviving because someone dug through a dusty closet. This isn’t healthcare. It’s a miracle economy.
-
Wren Hamley January 9, 2026
Wait-so the FDA requires 6-month advance notice but 47% of shortages stem from global supply chain fractures? That’s like requiring a weather forecast for a hurricane you can’t control. And if 83% of shortages are generics, why aren’t we subsidizing production like we do with vaccines or antibiotics? We treat these like commodities when they’re the bedrock of clinical care. The math is broken. The incentives are inverted. We’re not fixing this until we stop pretending it’s a logistics problem.
-
Philip Leth January 10, 2026
Man, this reminds me of when I was in the Army med unit. We used to hoard saline bags like gold. One time we had to use bottled water and salt to make IV fluid because the shipment got stuck at customs. That’s not science. That’s survival. We got lucky. Not everyone does. This ain’t just a US problem-it’s a global failure of prioritization.
-
Angela Goree January 11, 2026
THIS IS WHY WE NEED AMERICA TO MAKE AMERICAN DRUGS!!!
Why are we letting China and India control our medicine?!
It’s national security!!!
Our soldiers, our kids, our grandparents-all at risk because we outsource the basics!!!
WE NEED A MANUFACTURING REVIVAL!!!
NO MORE FOREIGN DEPENDENCE!!!
BUY AMERICAN OR DIE WITHOUT!!!
