
Breastfeeding Medication Timing Calculator
This tool helps you calculate the optimal time to take common medications to reduce infant exposure through breast milk. Based on pharmacokinetic data and ABM Protocol #21.
Recommended Timing
Please select a medication and enter the last breastfeeding time to see recommendations.
Pro Tip: Always nurse before taking medication whenever possible. This reduces infant exposure by up to 70% for many medications.
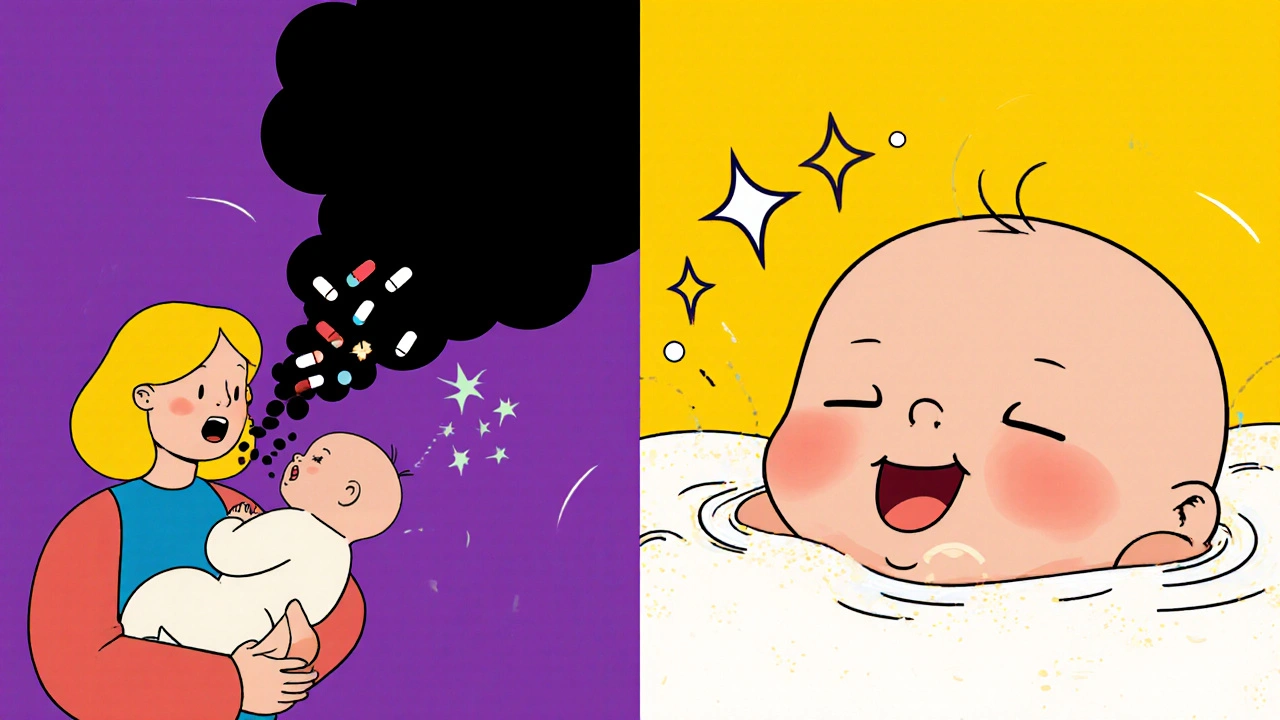
When you're breastfeeding and need to take medication, the last thing you want is to worry about your baby getting exposed to drugs through your milk. The good news? You don't have to choose between taking care of your health and keeping your baby safe. With the right timing, you can cut infant drug exposure by 50-75% for many common medications - without stopping breastfeeding.
Why Timing Matters More Than You Think
It’s not just about whether a drug is safe. It’s about when you take it. Medications enter your breast milk based on how much is in your bloodstream. That level peaks at different times depending on the drug. If you nurse right after taking a pill, your baby gets the highest dose. If you wait, the concentration drops - and so does their exposure. For example, if you take oxycodone, the drug hits peak levels in your blood between 30 minutes and 2 hours after swallowing it. If you breastfeed during that window, your baby gets more of the drug. But if you wait until 2-3 hours after taking it - when levels have started to fall - your baby’s exposure drops significantly. This isn’t guesswork. It’s backed by decades of pharmacokinetic research and formalized by the Academy of Breastfeeding Medicine (ABM) in their 2022 Protocol #21. Major organizations like the American Academy of Pediatrics, CDC, and AAFP all agree: timing is a proven, low-risk strategy that helps moms stay medicated and babies stay protected.How Much Drug Actually Gets to Your Baby?
Not all medications transfer equally. Scientists use something called the Relative Infant Dose (RID) to measure how much of the drug your baby actually gets through breast milk. It’s calculated as the amount your baby receives divided by your dose, adjusted for weight. An RID under 10% is generally considered safe. Here’s what real numbers look like:- Codeine: RID 0.6-8.1%
- Morphine: RID 9.0-35%
- Acetaminophen: RID less than 1%
- Ibuprofen: RID less than 1%
- Alprazolam (Xanax): RID around 5%
- Diazepam (Valium): RID up to 15% - but stays in milk for days
Which Medications Work Best With Timing?
Timing works best for drugs with short half-lives - meaning they leave your system quickly. Here’s how different classes stack up:Safe and Timing-Friendly
- Acetaminophen (Tylenol): Peaks in 30-60 minutes, half-life 2-4 hours. Breastfeed right before taking it.
- Ibuprofen (Advil): Peaks in 1-2 hours, half-life 2 hours. Very low transfer. Safe to take anytime, but best right after feeding.
- Hydrocodone: Peaks in 1-1.5 hours. Preferred over oxycodone. Wait 2-3 hours after taking it to nurse.
- Alprazolam: Peaks in 1-2 hours, half-life 11 hours. Timing helps reduce peak exposure.
Use With Caution - Timing Helps, But Doesn’t Fix Everything
- Morphine: High RID (up to 35%). Timing helps, but use lowest dose possible. Avoid in newborns.
- Tramadol: FDA warning due to unpredictable metabolism. Some babies get dangerously high levels even with timing. Not recommended.
- Codeine: FDA black box warning. Some people metabolize it too fast, turning it into dangerous levels of morphine. Avoid entirely.
- Diazepam: Half-life of 44-48 hours. Timing doesn’t matter much - it builds up. Use alternatives like lorazepam if possible.
Psychiatric Meds
For antidepressants and antipsychotics, immediate-release versions are key. Extended-release pills (like SSRIs with slow release) keep drug levels steady all day - making timing useless. If you’re on fluoxetine or sertraline, ask your doctor if you can switch to immediate-release forms for better control.When to Nurse - The Simple Rule
Here’s the easiest way to remember it:- Take your medication right after you breastfeed. This gives your body time to clear the drug before the next feeding.
- Wait 2-3 hours before the next nursing session. For most short-acting drugs, that’s enough time for levels to drop.
- For long-acting drugs (like diazepam), timing doesn’t help. Focus on using the lowest effective dose instead.
- For opioids, always nurse before taking the pill. This is the single most important step for safety.
What About Newborns and the First Few Days?
In the first 3-4 days after birth, your milk supply is low - colostrum, not mature milk. That means even if a drug is present, very little gets through. A 2023 Mayo Clinic review found that most medications transfer at negligible levels during this time. So if you’re on pain meds after delivery, don’t panic. Just keep an eye on your baby’s alertness and feeding. But don’t assume this safety lasts. By day 5, milk volume increases dramatically, and so does potential exposure.What If Your Baby Feeds Every 2 Hours?
Newborns don’t follow schedules. If your baby feeds every 90 minutes, waiting 2-3 hours between dose and feed isn’t always possible. Here’s how to handle it:- Pump and dump before taking your dose. Store the milk you pump before your medication. Use it for the next feeding. This is the most reliable method for unpredictable schedules.
- Use the lowest dose possible. Less drug in your system = less in your milk.
- Ask your doctor about alternatives. Some drugs have safer profiles even without timing.
- Don’t skip doses. Missing medication for your own health can be riskier than the drug exposure.
What Medications Should You Avoid Completely?
Timing won’t make these safe:- Codeine - FDA black box warning. Can turn into dangerous morphine levels in breastfed babies.
- Tramadol - Same risk. Unpredictable metabolism in moms and babies.
- Recreational drugs - Cocaine, heroin, marijuana - avoid entirely.
- Chemo drugs - Most are not compatible with breastfeeding. Consult an oncologist.
- Radioactive isotopes - Used in imaging. Must pause breastfeeding for hours or days depending on the tracer.
Where to Find Reliable Info - And Who to Ask
Don’t rely on Google or forums. Use trusted sources:- LactMed - A free database from the National Library of Medicine. Updated quarterly. Lists drugs, RID values, and timing tips.
- Academy of Breastfeeding Medicine (ABM) - Their clinical protocols are gold standard.
- La Leche League - Trained volunteers can help you interpret guidelines.
- Your pharmacist - Ask if they’ve checked LactMed. Most know how to access it.
- Your OB or pediatrician - If they don’t know about timing, ask them to consult a lactation specialist.
Real-Life Example: A Mom’s Story
Sarah, 32, had a C-section and was prescribed hydrocodone. She was terrified of hurting her 3-day-old. Her lactation consultant showed her the timing trick: nurse at 8 p.m., take the pill at 10 p.m., next feed at 1 a.m. That gave her 3 hours between dose and feeding. She also pumped and saved milk before her first dose. Within a week, she was sleeping through the night without fear. Her baby gained weight normally and showed no signs of drowsiness. Her secret? She didn’t stop breastfeeding. She just changed when she took the pill.Final Thoughts: You Can Do This
Breastfeeding while on medication isn’t about perfection. It’s about smart choices. You don’t need to go without pain relief, anxiety meds, or antibiotics. You just need to know when to take them. The science is clear: timing reduces exposure. The organizations agree: it’s safe and effective. The tools are available: LactMed, pharmacists, lactation consultants. And the goal is within reach: keeping your baby nourished, healthy, and close to you - while you take care of yourself.Frequently Asked Questions
Can I breastfeed after taking ibuprofen?
Yes. Ibuprofen transfers very little into breast milk - less than 1% of your dose. It’s one of the safest pain relievers for nursing moms. You can take it right after feeding and nurse again in 2-3 hours, but even if you nurse sooner, the amount your baby gets is minimal and safe.
Is it safe to take Tylenol while breastfeeding?
Absolutely. Acetaminophen (Tylenol) has an RID under 1%, meaning your baby gets almost nothing. It’s cleared from your system in 2-4 hours. You can take it anytime, but for maximum safety, take it right after nursing.
What if I take a medication and forget to time it?
Don’t panic. If you nursed right after taking a pill, skip the next feeding and pump and dump if you’re uncomfortable. Wait 2-3 hours, then nurse again. One missed timing window won’t harm your baby - especially with low-risk drugs. Consistency matters more than perfection.
Can I pump and dump to make breastfeeding safer?
Pumping and dumping only helps if you do it before taking the medication. Pumping after taking a drug won’t remove it from your system - the drug is still circulating in your blood. The only way to reduce exposure is to time your dose so your milk has less of it when you feed. Pumping before your dose and storing that milk for later is the best strategy.
Are herbal supplements safe while breastfeeding?
Many aren’t well studied. Things like chamomile or ginger are generally low risk, but others - like black cohosh, sage, or licorice root - can reduce milk supply or have unknown effects. Always check LactMed or ask a lactation specialist before taking any supplement, even if it’s labeled "natural."
Comments (9)
-
Kenneth Narvaez November 24, 2025
The pharmacokinetic principles outlined here are fundamentally sound, particularly the emphasis on peak plasma concentration windows and relative infant dose (RID) thresholds. For short-half-life NSAIDs like ibuprofen, the Cmax occurs at 1–2 hours post-ingestion with a serum half-life of approximately 2 hours, resulting in negligible transfer (<1%) to breast milk. The 2–3 hour post-dose nursing interval aligns with the elimination phase, reducing infant exposure by 50–75% as cited in ABM Protocol #21. This is not anecdotal-it's rooted in linear pharmacokinetic modeling validated across multiple clinical studies.
-
Christian Mutti November 26, 2025
I must express my profound concern regarding the casual dismissal of pharmacological risk in this post. While the data may appear reassuring, we are speaking of neonatal neurodevelopment-where even microdoses of opioids or benzodiazepines can have irreversible consequences. The FDA’s black box warnings on codeine and tramadol exist for a reason. To suggest that "timing" mitigates all risk is dangerously reductive. What of the infant with CYP2D6 ultra-rapid metabolism? What of the undiagnosed mitochondrial disorder? This is not a checklist-it’s a minefield.
-
Liliana Lawrence November 27, 2025
OMG, this is SO important!! 🙌 I just had my second baby and was terrified of taking anything-even Tylenol-until I found LactMed. Seriously, I cried reading the RID values. Like, acetaminophen is under 1%?! I felt like I’d been lied to my whole life. Also, pump before you dose?? Genius. I started doing that and now I nap without guilt. Thank you for this. My baby is thriving. 🥹💕
-
Sharmita Datta November 29, 2025
Are you aware that the FDA and CDC are part of a pharmaceutical conspiracy to normalize drug exposure in infants? The "RID" metric is fabricated by Big Pharma to sell more pills. Real mothers in the 1950s breastfed while taking aspirin and never had problems. Now they want you to pump and dump? That’s not medicine-it’s corporate control. The real danger is not the drug-it’s the fear they’ve implanted in you. Trust your body. Avoid all meds. Eat raw garlic. Pray. The system is rigged.
-
mona gabriel November 30, 2025
Timing isn’t magic. It’s math. And math doesn’t care if you’re tired or your baby screams every 90 minutes. I took hydrocodone after my C-section. My baby fed every 1.5 hours. I pumped before my first dose, stored it, and used it for the next feed. Didn’t stop nursing. Didn’t panic. Just worked with the system. The science is solid. The fear? That’s the noise. You’re not failing if you need meds. You’re just learning how to use them wisely.
-
Phillip Gerringer December 1, 2025
Let’s be clear: if you’re taking alprazolam while breastfeeding, you’re not a good mother. You’re self-medicating anxiety with a drug that accumulates in neonatal tissue. The fact that you’re looking for loopholes like "timing" instead of seeking therapy or non-pharmacological solutions speaks volumes. This isn’t about safety-it’s about convenience. Real mothers endure. They don’t chemically sedate themselves and then justify it with pharmacokinetics.
-
jeff melvin December 3, 2025
Hydrocodone over oxycodone? That’s just semantics. Both are opioids. Both cross the BBB. Both suppress respiration in neonates. The ABM guidelines are outdated. The 2023 AAP policy statement explicitly recommends avoiding all opioids in the first 72 hours postpartum. Period. No timing tricks. No exceptions. If you need pain control, use ice, physical therapy, or acetaminophen. Anything else is gambling with your child’s life.
-
Matt Webster December 4, 2025
I just want to say: you’re not alone. I was terrified when I had to take sertraline after postpartum depression. I spent weeks reading LactMed, talking to my pharmacist, and working with a lactation consultant. I switched to immediate-release because my doctor listened. My baby is now 18 months old, thriving, and I’m finally sleeping. It’s okay to need help. It’s okay to take meds. It’s okay to ask for better care. You’re doing better than you think.
-
Stephen Wark December 5, 2025
This whole post is just corporate propaganda dressed up as science. They want you to keep breastfeeding so they can sell you more drugs. Meanwhile, real moms are being told to pump and dump while their babies cry from withdrawal. Who benefits? The hospitals. The pharmacies. The drug companies. Not you. Not your baby. Stop trusting the system. Go herbal. Go raw. Go primal. Or better yet-stop breastfeeding. It’s not worth it.
