Acid reflux: fast facts and real fixes
Acid reflux happens when stomach acid pushes up into your esophagus and causes that familiar burn or sour taste. Sometimes it's occasional heartburn after a big meal. Other times it becomes GERD — chronic reflux that needs treatment. This guide gives straight, useful steps you can try today and explains when to see a doctor.
What brings it on (and what to avoid)
Common triggers are fatty or fried foods, chocolate, peppermint, caffeine, alcohol, citrus, tomato-based dishes, and large late meals. Smoking and obesity make reflux worse because they relax the valve (lower esophageal sphincter) that keeps stomach acid down. Lying flat right after eating or eating too quickly also raises the risk.
If you have diabetes, mention it to your clinician — delayed stomach emptying (gastroparesis) can look like reflux but needs different care.
Quick fixes and medicines
For fast relief try an antacid (Tums, Maalox) to neutralize acid. They work right away but wear off quickly. H2 blockers (famotidine, ranitidine alternatives) reduce acid for several hours and can help mild, repeat heartburn. Proton pump inhibitors (PPIs) like omeprazole or esomeprazole cut acid production more strongly and are the go-to for frequent reflux — but use them under a doctor’s guidance if you need them longer than a few weeks.
A note on prokinetics: drugs such as metoclopramide may be used to speed stomach emptying, but they can have mental side effects and other risks, so they’re not first-line for everyone. Always talk to your doctor about side effects and interactions, especially if you take other meds.
Non-prescription options help many people, but if symptoms return as soon as you stop pills, you need a medical review.
Simple lifestyle moves make a big difference. Lose even a little weight if you’re overweight — many people feel much better with a 5–10% bodyweight drop. Eat smaller meals and stop eating at least 2–3 hours before bed. Raise the head of your bed 6–8 inches or use a wedge pillow so gravity keeps acid down while you sleep. Quit smoking and cut back on alcohol and caffeine. Wear loose clothes around your waist.
If symptoms include trouble swallowing, unintentional weight loss, vomiting, bloody or black stools, or persistent chest pain, get medical help fast. Tests like endoscopy or pH monitoring can identify damage, rule out other problems, and guide treatment.
Realistic plan: try diet and sleep changes for 2–4 weeks, use antacids as needed, move to an H2 blocker if symptoms keep coming, and see a clinician before starting long-term PPIs. Keep a simple symptom log (what you ate, when symptoms started) to share with your provider — it speeds diagnosis and gets you the right fix sooner.
Want help picking an over-the-counter option or checking drug interactions with your current meds? Reach out to your pharmacist or healthcare provider — they can tailor advice to your health profile and keep things safe.
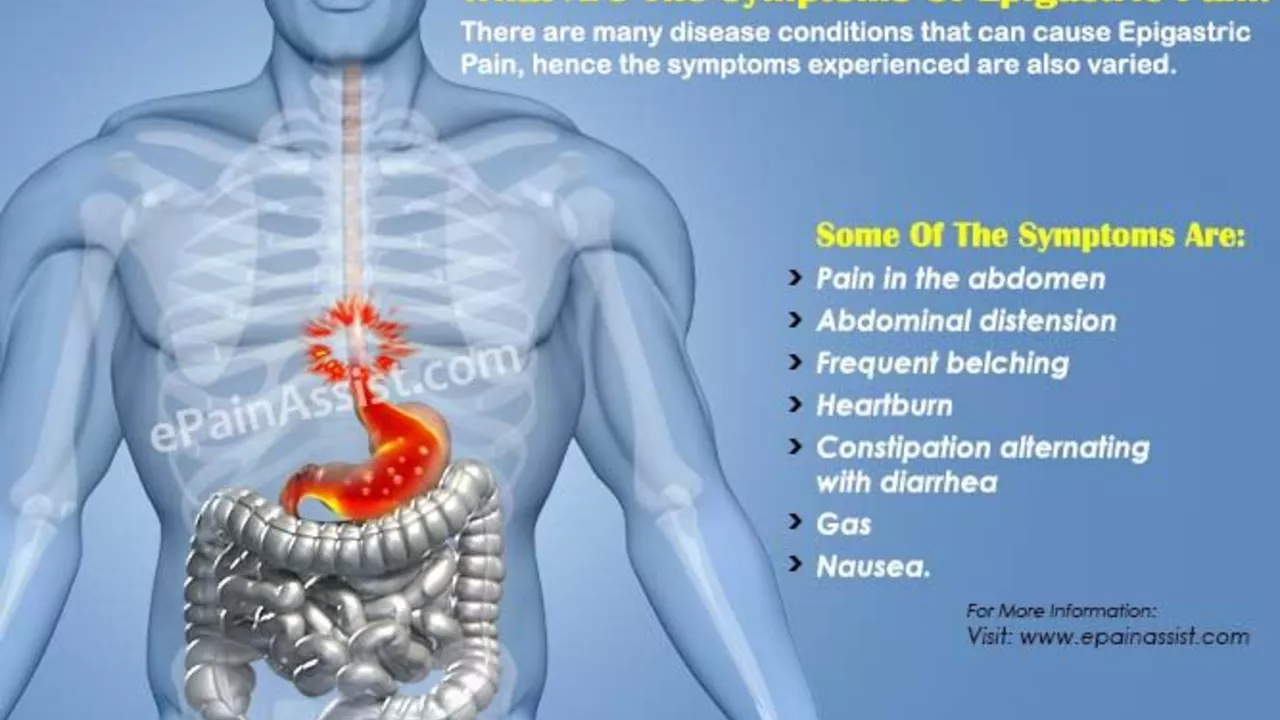
Epigastric Pain and Acid Reflux: Tips for Managing Symptoms
Haig Sandavol Aug 1 14Belly battles are no fun, mate! Epigastric pain and acid reflux, the dynamic duo of discomfort, often go hand in hand. But don't panic, I've got some handy tips to help you fight back. From dietary changes to lifestyle modifications, there are several tactics you can employ to keep these pesky problems in check. So, sit tight, as we dive into the world of managing these fiery foes, promising a smoother journey down your food pipe!
More Detail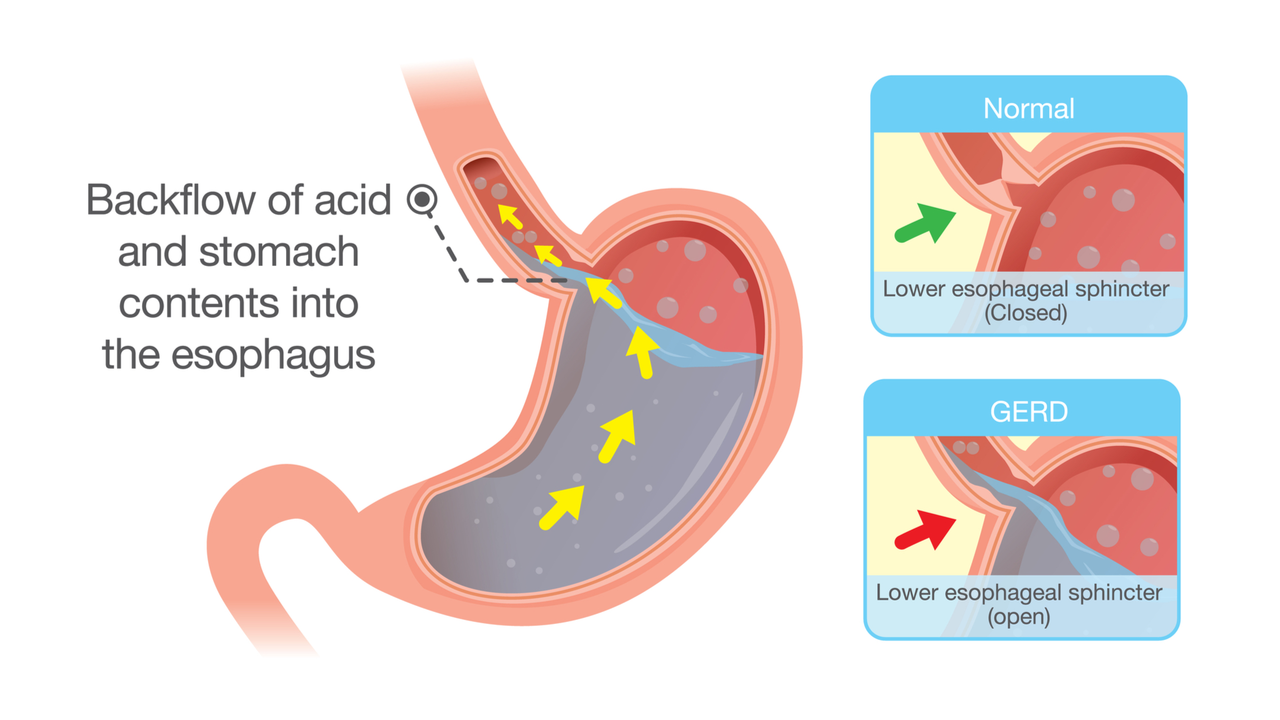
GERD and Acid Reflux: Understanding the Differences Between These Digestive Disorders
Haig Sandavol Jun 12 6As a blogger, I've come to realize the importance of understanding the differences between GERD and acid reflux, two common digestive disorders. While both involve stomach acid flowing back into the esophagus, GERD is a chronic condition characterized by frequent acid reflux episodes. Acid reflux, on the other hand, is an occasional occurrence that can be triggered by certain foods or lifestyle factors. By being aware of these distinctions, we can better manage our digestive health and seek appropriate treatment when necessary. Stay tuned for more insights on these conditions and how to keep them in check!
More Detail