
For millions of low-income Americans on Medicaid, the difference between a generic pill and a brand-name one isn’t just about the label-it’s about whether they can afford to take it at all. In 2023, Medicaid generics filled 90% of all prescriptions under the program, but they made up less than 18% of the total drug spending. That’s not a coincidence. It’s the result of a system built to stretch every dollar for people who can’t afford to pay full price.
Why Generics Are the Backbone of Medicaid
Medicaid doesn’t just cover low-income patients-it’s designed to keep them healthy without bankrupting them. And generics are the reason it works. When a doctor prescribes a medication, Medicaid’s pharmacy system automatically fills it with the generic version unless there’s a medical reason not to. That’s not a restriction-it’s a feature. The generic version of a drug has the same active ingredients, the same effectiveness, and the same safety profile as the brand-name version. The only difference? The price. In 2023, the average copay for a generic drug under Medicaid was $6.16. For a brand-name drug? $56.12. That’s nearly nine times more. For someone living paycheck to paycheck, that difference means choosing between medicine and groceries. Generics make the impossible, possible.How Medicaid Gets Such Low Prices
Medicaid doesn’t just rely on competition between drugmakers to keep prices down. It has a powerful tool: the Medicaid Drug Rebate Program (MDRP). Created in 1990, this rule forces drug companies to give back a big chunk of what they charge Medicaid. For most generic drugs, the rebate is around 86% of the retail price. That means if a generic costs $10 at the pharmacy, Medicaid pays less than $1.50 after the rebate. In 2023, these rebates saved the program $53.7 billion-over half of what was spent on drugs before rebates. That’s more than the entire annual budget of many U.S. states. Medicaid gets better prices than even the Department of Veterans Affairs, which is known for its aggressive pricing. And it’s not just about volume. Because Medicaid covers so many people, it has leverage that private insurers don’t.The Hidden Cost: Pharmacy Benefit Managers (PBMs)
But here’s the catch: not all the savings make it to the patient. A big slice of the money gets eaten up by Pharmacy Benefit Managers-middlemen hired by states to manage drug benefits. In Ohio, a 2025 audit found that PBMs took 31% of the cost on $208 million worth of generic drugs in just one year. That’s $64 million in fees on drugs meant to be cheap. These fees don’t show up on your receipt. You won’t see them on your Medicaid card. But they’re there, reducing the savings that should go to patients and taxpayers. Some states are starting to push back-requiring more transparency and capping PBM fees. But nationally, the system still favors intermediaries over the people who need the drugs most.
Generics vs. Brand-Name: The Real Numbers
It’s easy to say generics save money. But the numbers tell the real story:- 90-91% of Medicaid prescriptions are for generics
- Generics account for only 17.5-18.2% of total Medicaid drug spending
- 93% of generic prescriptions cost less than $20 at the pharmacy counter
- Only 59% of brand-name prescriptions cost under $20
- The average generic copay: $6.16
- The average brand-name copay: $56.12
What’s Making Drug Costs Rise Anyway?
If generics are so cheap, why is Medicaid spending on drugs still going up? The answer isn’t generics. It’s specialty drugs. Less than 2% of Medicaid prescriptions are for drugs that cost over $1,000 per claim. But those few drugs account for more than half of all Medicaid drug spending. Think cancer treatments, rare disease therapies, and biologics. These aren’t generics. They’re expensive, complex, and often without competition. Net Medicaid drug spending jumped from $30 billion in 2017 to $60 billion in 2024. That’s a 100% increase in just seven years. And while generics are still filling 90% of prescriptions, the cost of those few high-price drugs is pulling the whole system up. That’s why CMS launched the GENEROUS Model in 2024-to find ways to control spending on these specialty drugs without cutting access.What Patients Actually Experience
Real people don’t care about rebate percentages or PBM fees. They care about whether they can pick up their medication without stress. A mother in Texas told her story on a Medicaid support forum: “My son’s ADHD medication switched from brand to generic. My copay dropped from $25 to $4. I cried in the pharmacy line. I hadn’t realized how much I was stressing over that $25 every month.” But it’s not always smooth. Some patients face delays. One Reddit user wrote: “My daughter’s asthma inhaler was switched to generic. Copay went from $25 to $3. But it took three weeks and six phone calls to get approval.” That’s the downside of prior authorization-a system meant to prevent overuse but often becomes a barrier. States vary widely in how they handle these rules. Some have streamlined systems. Others require paperwork that feels designed to discourage people from getting help. The National Association of Medicaid Directors gave state transparency a 7.2 out of 10 in 2024. That means nearly a third of patients are left guessing what’s covered and why.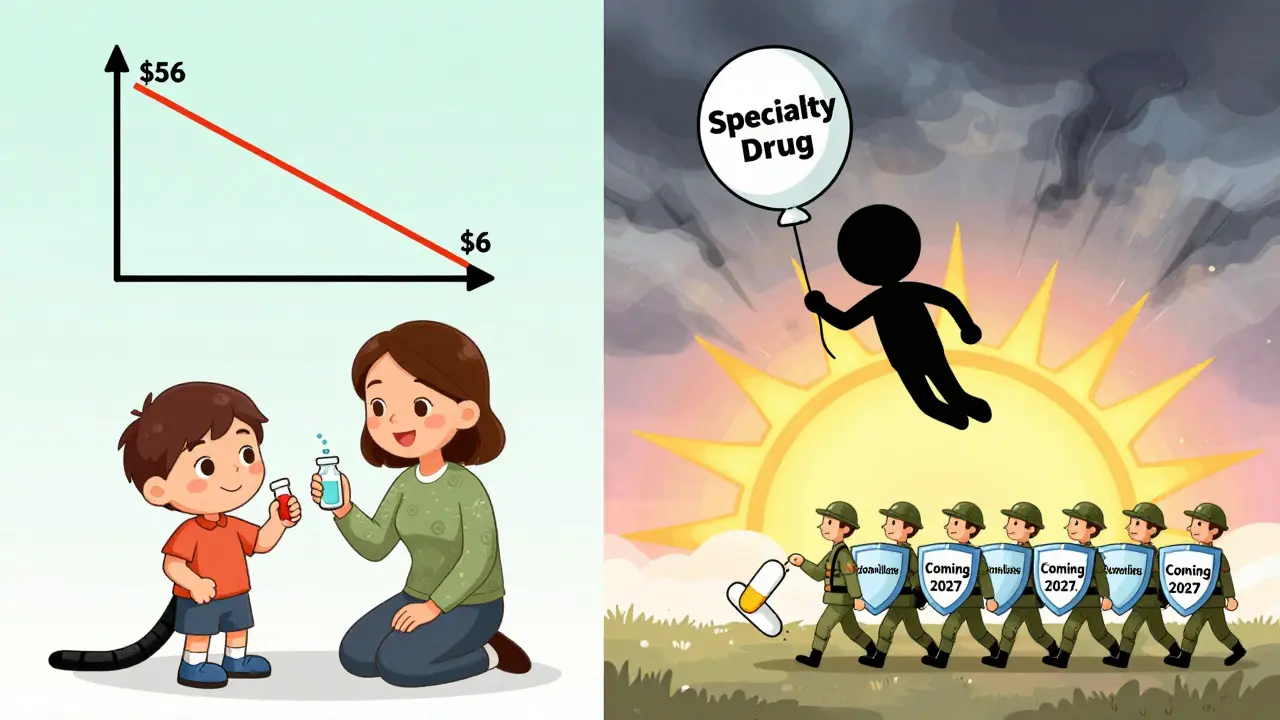
What You Can Do as a Medicaid Beneficiary
You don’t need to be a policy expert to get the most out of your coverage. Here’s what works:- Always ask if a generic is available-even if your doctor prescribes a brand name. Pharmacists can substitute unless the doctor says no.
- Know your state’s formulary. Some states have tiered copays. Generics are almost always Tier 1-the lowest cost.
- Use mail-order pharmacies if available. Many states offer 90-day supplies of generics for the same copay as a 30-day fill.
- Call your state’s Medicaid office if you’re denied a drug. You have the right to appeal.
- Check if your pharmacy offers a discount card. Some generic drugs cost less through manufacturer coupons than through Medicaid.
The Bigger Picture: Generics Are a National Success Story
Since 2009, generic drugs have saved the U.S. healthcare system $2.2 trillion. In 2022 alone, they saved $408 billion. That’s not just Medicaid’s win-it’s every taxpayer’s win. For low-income families, it’s life-changing. The system isn’t perfect. PBMs take too much. Specialty drugs are a growing problem. Some states make it harder than it should be to get your meds. But the core idea-using generics to keep people healthy without breaking the bank-works better than any other part of the system. As more biologic drugs lose patent protection over the next few years, biosimilars-generic versions of complex biologic drugs-could save Medicaid another $100 billion a year by 2027. That’s the next frontier. And it’s one worth fighting for.What’s Next for Medicaid and Generics?
The future of Medicaid drug spending depends on two things: keeping generics affordable and controlling the cost of specialty drugs. The GENEROUS Model is a start. So is the Inflation Reduction Act, which lets Medicare negotiate drug prices. Experts believe if those same rules applied to Medicaid, the program could save $15-20 billion over the next decade. But none of that matters if patients can’t get their meds. The real measure of success isn’t how much money Medicaid saves-it’s how many people are taking their pills every day. And right now, thanks to generics, millions are.Are generic drugs as safe and effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredients, strength, dosage form, and route of administration as the brand-name version. They must also meet the same strict standards for quality, purity, and performance. Studies show generics work just as well. The only differences are in inactive ingredients like fillers or colorants, which don’t affect how the drug works in your body.
Why is my generic drug copay higher than I expected?
Sometimes, state Medicaid programs increase copays even when the drug’s price drops. This can happen due to budget pressures or PBM fee structures. If your copay seems too high, ask your pharmacy if the drug is listed on your state’s formulary. You can also call your state’s Medicaid office to report the issue-many states have programs to cap or reduce copays for low-income patients.
Can I get my generic medication cheaper without Medicaid?
Sometimes, yes. Programs like the Mark Cuban Cost Plus Drug Company offer some generics at lower prices than insurance copays. But these are usually limited to a small selection of drugs-only about 26% of common generics are available. For most people on Medicaid, the program still offers the best overall price, especially when rebates and low copays are factored in.
Why does Medicaid require prior authorization for some generics?
Prior authorization is meant to prevent overuse or misuse, but it’s often applied inconsistently. Some states require it for certain generics if they’re newer or if there’s a brand-name version still on the market. It’s not about cost-it’s about control. If you’re denied, you have the right to appeal. Keep records of all calls and paperwork. Many denials are overturned with a simple phone call.
Do all states offer the same generic drug coverage under Medicaid?
No. While federal law requires Medicaid to cover all medically necessary drugs, each state sets its own formulary, copay amounts, and prior authorization rules. Most states cover the same core generics, but availability of newer generics can vary. Some states update their lists monthly; others take months or years. Always check your state’s official Medicaid website or call their helpline for the most accurate info.
Comments (10)
-
Lydia H. January 20, 2026
It’s wild how something so simple-switching to generics-can turn a monthly crisis into a sigh of relief. I’ve seen friends choose between insulin and rent, and generics? They’re the quiet hero nobody talks about. No fanfare, no headlines. Just a $4 copay keeping someone alive.
-
Jacob Hill January 22, 2026
Let me just say: PBMs are the real villains here. They’re not pharmacists, they’re not doctors-they’re corporate middlemen who take a cut from every $1.50 Medicaid pays for a generic. And they hide behind ‘administrative fees’ like it’s a technicality. It’s not. It’s theft dressed up as logistics.
-
Jackson Doughart January 22, 2026
The data is undeniable. Generics aren’t just cost-effective-they’re ethically necessary. When a child with asthma can breathe because their inhaler costs $3 instead of $25, that’s not policy. That’s dignity. And we should treat it as such.
-
Lewis Yeaple January 24, 2026
While the narrative around generics is largely accurate, it is imperative to acknowledge that the FDA’s bioequivalence standards permit a 20% variance in absorption rates-this is not trivial for patients on narrow-therapeutic-index drugs such as warfarin or levothyroxine. Therefore, blanket substitution without clinician oversight may, in rare but critical cases, pose clinical risk.
-
sujit paul January 24, 2026
Do you realize that the entire Medicaid generic system is a trap? The government lets drug companies sell generics at pennies, then takes the savings and gives it to PBMs and bureaucrats. Meanwhile, real people still wait weeks for prescriptions. This isn’t care-it’s control. The elite don’t want you healthy. They want you dependent.
-
Christi Steinbeck January 25, 2026
If you’re on Medicaid and you’re not asking your pharmacist if there’s a cheaper generic-YOU’RE LEAVING MONEY ON THE TABLE. Seriously. I helped my aunt get her blood pressure med down from $35 to $2 using a coupon and a 90-day mail order. It’s not magic. It’s knowing your rights.
-
Tracy Howard January 26, 2026
It’s laughable how Americans act like Medicaid is some noble achievement. Meanwhile, in Canada, we get all prescriptions for under $5-no rebates, no PBMs, no forms. You don’t need a PhD in healthcare policy to understand that universal coverage just… works. Stop patting yourselves on the back for barely scraping by.
-
Jake Rudin January 27, 2026
It’s worth noting that the 90% generic fill rate is misleading-it doesn’t account for the fact that many patients are prescribed brand-name drugs first, then forced to go through prior authorization to switch. The system is designed to create friction. The numbers look good on paper, but the lived experience? That’s where the real failure lies.
-
Astha Jain January 29, 2026
generics r fine but why do u always have 2 wait 3 weeks for em? its like the system wants u 2 give up… also my doc said brand only but pharmacy swapped it anyway… now i feel weird takin it 😅
-
Erwin Kodiat January 29, 2026
I’m from the Midwest, and I’ve seen this firsthand. My neighbor’s kid with epilepsy was on a brand-name med that cost $180 a month. Switched to generic-copay dropped to $5. Kid’s been seizure-free for two years. That’s not a statistic. That’s a life. We don’t need to fix everything. We just need to protect what’s already working.
