
Ear Infection Hearing Risk Calculator
This tool assesses your risk of hearing loss from ear infections based on factors discussed in the article. Enter your information below to receive personalized recommendations.
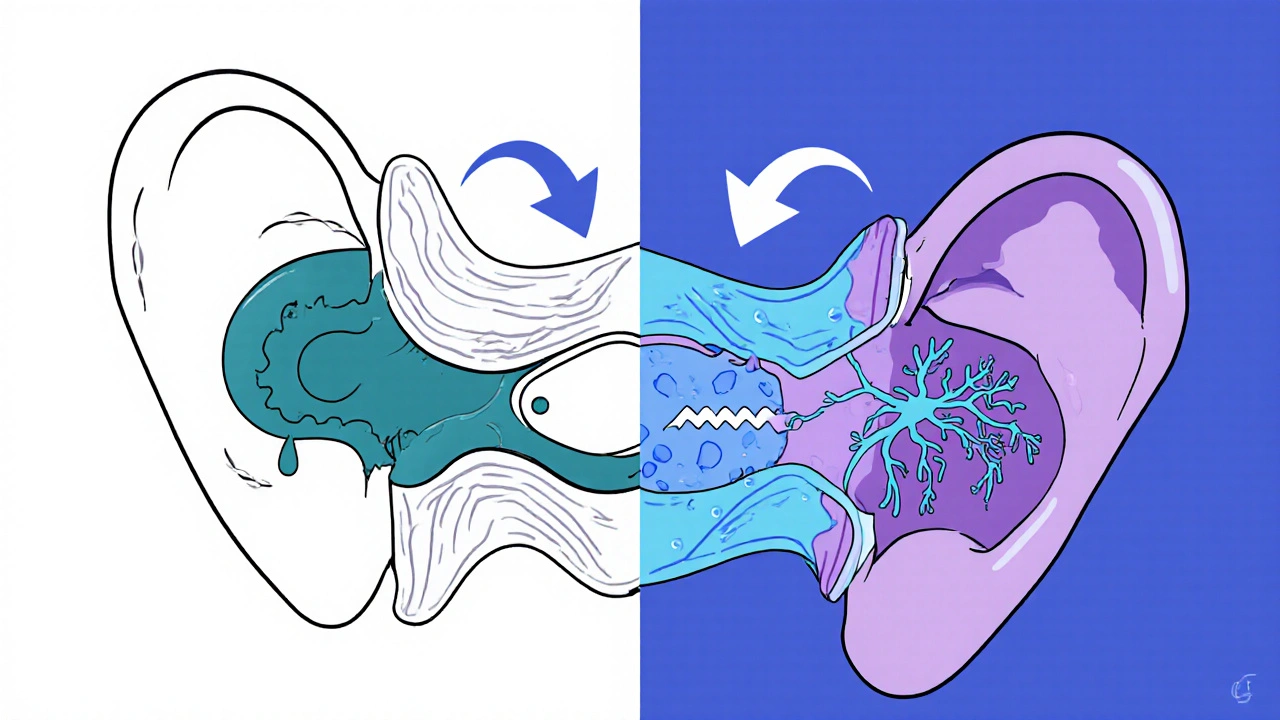
Ear Infections are inflammation of the middle ear, most commonly caused by bacteria or viruses that travel up the Eustachian Tube. When fluid builds up and the ear cannot ventilate properly, pressure changes can damage delicate structures, setting the stage for Hearing Loss. This article explains how the two are connected, who’s most at risk, and what steps can stop permanent damage.
Why Ear Infections Matter for Your Auditory System
The middle ear houses the tiny ossicles-malleus, incus, and stapes-that transmit sound vibrations to the inner ear. An infection (often called Otitis Media) fills the cavity with fluid, limiting ossicle movement. Repeated fluid buildup creates a chronic environment that can erode the bones and the round window, leading to Conductive Hearing Loss. In children, the eardrum (tympanic membrane) is thinner, so even short‑term infections can cause scarring-known as tympanosclerosis-that permanently blocks sound transmission.
Types of Hearing Loss Linked to Ear Infections
While most ear infections cause conductive loss, severe or untreated cases can also affect the inner ear, resulting in Sensorineural Hearing Loss. The inner ear’s hair cells are highly sensitive to inflammation; bacterial toxins or viral replication can damage them, reducing the ear’s ability to convert vibrations into electrical signals.
| Aspect | Conductive | Sensorineural |
|---|---|---|
| Primary Site | Middle ear ossicles or eardrum | Inner ear hair cells or auditory nerve |
| Typical Cause | Fluid buildup, otitis media, tympanostomy tubes | Viral infection, prolonged inflammation, genetic factors |
| Reversibility | Often reversible with medical treatment | Usually permanent |
| Treatment Options | Antibiotics, tympanostomy tubes, decongestants | Hearing aids, cochlear implants, auditory rehab |
Who Is Most Susceptible?
Children under five bear the highest burden. Their Eustachian tubes are shorter and more horizontal, making drainage difficult. According to the World Health Organization (WHO), about 30% of children experience at least one episode of acute otitis media before age three. Premature infants, kids with cleft palate, and those exposed to second‑hand smoke also have elevated risk. Adults with chronic sinus issues or allergies can develop infections that eventually lead to hearing loss, especially when infections recur over years.
How Doctors Diagnose the Connection
A thorough evaluation begins with a pediatrician or an ENT specialist who uses an otoscope to inspect the eardrum. If fluid is present, a tympanogram measures ear pressure. For suspected inner‑ear involvement, an Audiogram quantifies hearing thresholds across frequencies. In chronic cases, a CT scan may reveal ossicle erosion. Early detection is critical-studies from 2023 show that children who receive timely treatment for otitis media have a 40% lower chance of developing measurable hearing loss by age ten.
Treatment Pathways That Protect Hearing
Acute infections often respond to a short course of antibiotics, especially when bacterial pathogens like Streptococcus pneumoniae are identified. However, overuse of antibiotics can foster resistance, so doctors may first recommend watchful waiting. For recurrent cases, Tympanostomy Tubes-tiny ventilation tubes placed in the eardrum-allow fluid to drain and equalize pressure. The procedure has a success rate above 80% for preventing long‑term conductive loss. Adjunct therapies include nasal steroids for allergy‑related congestion and oral decongestants in short bursts.

Practical Steps to Reduce Risk
- Breastfeed infants for at least six months. Breast milk contains antibodies that lower infection rates.
- Keep vaccinations up to date-especially the pneumococcal and influenza vaccines, which cut otitis media incidents by ~20%.
- Avoid exposing children to cigarette smoke; second‑hand smoke doubles infection risk.
- Practice good hand hygiene during cold and flu season to limit viral spread.
- Schedule regular hearing screenings for children with a history of three or more ear infections.
When to Seek Immediate Care
If an ear infection is accompanied by severe pain, fever over 101°F (38.3°C), drainage of pus, or sudden hearing loss, medical attention is urgent. Persistent discharge may indicate a perforated eardrum, which requires specialist intervention to prevent chronic conductive loss.
Frequently Asked Questions
Can a single ear infection cause permanent hearing loss?
Rarely. Most single episodes resolve without lasting damage, especially if treated promptly. The risk rises with repeated infections or if fluid remains for more than three months.
What’s the difference between conductive and sensorineural hearing loss?
Conductive loss blocks sound from reaching the inner ear, often due to fluid or eardrum damage. Sensorineural loss stems from damage to the inner ear hair cells or auditory nerve, usually permanent.
Are antibiotics always needed for ear infections?
Not always. Many infections are viral and resolve on their own. Doctors weigh factors like age, severity, and risk of complications before prescribing.
How long do tympanostomy tubes stay in the ear?
Typically 6‑12 months before they naturally extrude. Some children may need a second set if infections persist.
Can adults develop hearing loss from ear infections?
Yes, especially if infections are chronic or if underlying conditions like allergies or diabetes are present. The impact is often less severe than in children but still significant.
Comments (14)
-
Joe Moore October 18, 2025
Yo, they dont want ya to know this but every time you get a "simple" ear infection they push a miracle antibiotic that scratches the inner ear just enough to keep the pharma $$$ flowing. The CDC's *real* agenda is to keep the public hooked on meds while they hide the real cure in plain sight. Stay woke, read the label upside down, and never trust a doctor who says "just take two of these".
-
Emma Williams October 27, 2025
Thanks for the thorough breakdown, really helpful
-
Drew Waggoner November 5, 2025
Reading this just makes me feel the weight of all those kids suffering in silence while their parents brush it off as "just a cold". The constant cycle of fear and hope is exhausting, and it reminds me of how fragile our sense of normalcy truly is.
-
Ayla Stewart November 14, 2025
I get why some folks are skeptical, but the medical community does have solid data showing that untreated otitis media can lead to lasting conductive loss. Early intervention, like proper monitoring and ventilation tubes, really does help prevent those outcomes.
-
Poornima Ganesan November 22, 2025
Honestly, if you think a single paragraph summary captures the nuance of otologic pathology, you're missing the forest for the trees; the interplay between bacterial virulence factors, host immune responses, and the delicate architecture of the ossicular chain is far more complex than a quick "thanks". Moreover, the literature from the past decade consistently emphasizes that delayed audiometric screening in high‑risk infants increases the odds of permanent sensorineural deficits by a staggering margin, a fact that many laypeople simply overlook.
-
James Mali December 1, 2025
Another thing to consider is that just because an infection is labeled "acute" doesn't mean it won't have lingering effects on auditory processing. The philosophical side of it is that we often chase quick fixes, ignoring the long‑term integrity of our hearing apparatus. 😊
-
Mike Hamilton December 10, 2025
yeah, i think u r right, but also we gotta look at this from a cultural angle. many families see ear infections as just a rite of rite of passing childhood, and they might delay treatment cuz they think it's normal. this kind of mindset can lead to big problems later on, especially in communities with less access to ENT care.
-
Karla Johnson December 19, 2025
Ear infections are more than just a nuisance; they are a silent threat that can shape a child's auditory future in ways many parents never anticipate. When fluid accumulates in the middle ear, it creates a moist environment where bacteria multiply, and the resulting inflammation can erode the delicate ossicular chain that transmits sound. The longer this fluid remains, the higher the chance that scar tissue will form on the eardrum, a condition known as tympanosclerosis, which can permanently block sound waves. Moreover, the inner ear's hair cells, which are essential for converting vibrations into neural signals, are highly susceptible to damage from bacterial toxins and viral particles that may seep through the round window. Repeated bouts of otitis media can thus transition a primarily conductive loss into a mixed or even sensorineural loss, complicating treatment options. Studies have shown that children who receive timely antibiotics and, when necessary, tympanostomy tubes, recover hearing levels comparable to their peers within weeks. However, overreliance on antibiotics can lead to resistance, making future infections harder to manage and potentially more damaging. It's also crucial to recognize environmental risk factors; exposure to second‑hand smoke, for instance, doubles the incidence of middle‑ear infections in toddlers. Breastfeeding for at least six months provides immunoglobulins that significantly lower infection rates, acting as a natural preventive measure. Vaccinations, particularly against Streptococcus pneumoniae and influenza, shave off roughly twenty percent of otitis media cases, further reducing the burden on the auditory system. Parents should stay vigilant for signs like persistent ear pain, fluid drainage, or sudden changes in a child's responsiveness to sound, and seek professional evaluation promptly. Regular hearing screenings, especially for children with a history of three or more infections, can catch subtle deficits before they become entrenched. While surgical interventions like tympanostomy tubes have an success rate exceeding eighty percent in preventing long‑term conductive loss, they are not without risks, such as tube blockage or perforation of the eardrum. Ultimately, the key lies in a balanced approach that marries preventive care, judicious medical treatment, and early detection to safeguard hearing health. By taking these steps, families can dramatically reduce the likelihood that a common childhood ear infection translates into a lifelong hearing challenge.
-
Albert Fernàndez Chacón December 28, 2025
Totally see where you're coming from; the data you laid out aligns with the audiology community's push for early screening, and the jargon around "ossicular erosion" really hits home for clinicians.
-
Matthew Miller January 6, 2026
Whoa, this info is pure gold! Let's keep spreading the word-every parent needs to know the stakes and act fast. 🚀
-
Alex Lineses January 14, 2026
Great enthusiasm! If you're looking to share resources, the American Academy of Pediatrics has a solid toolkit for parents on recognizing otitis media signs and steps to take.
-
Brian Van Horne January 23, 2026
In summary, prompt identification and appropriate management of otitis media are essential to mitigate the risk of subsequent auditory impairment.
-
Janet Morales February 1, 2026
Honestly, that's just the tip of the iceberg-most people act like a quick summary will stop the avalanche of hearing loss looming over our kids, but the reality is far messier and more urgent.
-
Rajesh Singh February 10, 2026
While your frustration is understandable, it's vital to remember that we have a moral responsibility to advocate for evidence‑based interventions rather than succumb to fatalistic attitudes that ignore the plight of vulnerable children.
