
Every year, more than 1.2 million people in the U.S. end up in emergency rooms because of medication overdoses. Many of these cases involve common drugs-painkillers, sleep aids, antidepressants-that people take as prescribed but accidentally take too much. Or worse, they’re taken intentionally. The good news? For several of the most dangerous overdoses, there are specific antidotes that can save your life-if you act fast and know what to do.
What an Antidote Actually Does
An antidote isn’t just a pill that makes you feel better. It’s a targeted treatment that works at the chemical level to undo the poison. Think of it like a key that fits only one lock. Naloxone unlocks opioid receptors to reverse breathing slowdown. N-acetylcysteine (NAC) rebuilds liver defenses after acetaminophen overload. Flumazenil blocks the calming effect of benzodiazepines so your brain can wake up again. These aren’t general treatments-they’re precise tools used in emergencies.They don’t replace calling 911. They don’t replace fluids, oxygen, or monitoring. But when used correctly, they can be the difference between full recovery and permanent damage-or death.
Naloxone: The Opioid Overdose Reversal Tool
Opioid overdoses-from prescription pain pills, heroin, or fentanyl-are the leading cause of overdose deaths in the U.S. The signs are clear: slow or stopped breathing, blue lips, unresponsiveness, pinpoint pupils.Naloxone is the antidote. It works in minutes. You can get it as a nasal spray (like Narcan) or an auto-injector. The standard dose is 0.4 mg to 2 mg, given either in the nose or muscle. If there’s no response after 2-3 minutes, give another dose. Some people need two or three doses because fentanyl is so strong.
Here’s what most people don’t realize: naloxone wears off in 30 to 90 minutes. Opioids can stay in your system much longer. So even if you wake someone up, you still need to call 911. They could slip back into overdose once the naloxone wears off.
Since 2023, Narcan nasal spray is available over-the-counter at pharmacies without a prescription in all 50 states. Many community centers, libraries, and harm reduction programs give it away for free. If you or someone you know uses opioids-even if it’s just for pain-you should have naloxone on hand. Keep it in your bag, your car, your medicine cabinet. It’s not just for addicts. It’s for anyone who might accidentally take too much.
N-Acetylcysteine (NAC): Saving the Liver After Acetaminophen Overdose
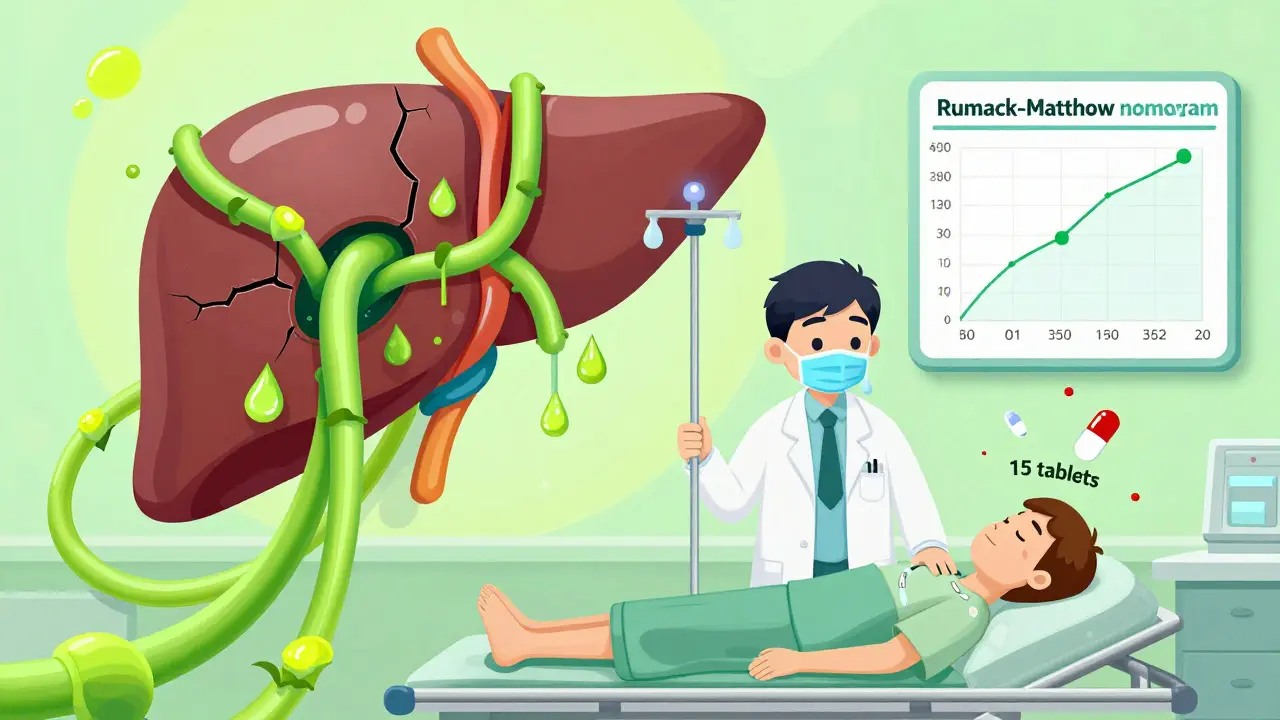
Acetaminophen-Tylenol-is one of the most common drugs found in overdose cases. It’s in hundreds of cold and pain medicines. People think it’s safe because it’s sold over the counter. But 15 pills can kill your liver.The problem? You won’t feel sick right away. For the first 12 to 24 hours, you might feel fine. That’s when people delay going to the hospital. But by the time nausea, vomiting, or jaundice shows up, the damage is already spreading.
NAC is the antidote. It’s given intravenously in a hospital over 21 hours, or orally as a bitter-tasting liquid. The key is timing. If you get NAC within 8 hours of taking too much acetaminophen, the chances of avoiding liver failure are over 98%. After 16 hours, that drops sharply. After 24 hours, it’s often too late.
Doctors use a blood test called the Rumack-Matthew nomogram to decide if you need NAC. It plots your acetaminophen level against the time since ingestion. If you’re unsure how much you took, or if it was mixed with alcohol or other meds, get checked anyway. Don’t wait for symptoms. Liver damage doesn’t hurt until it’s too late.
Flumazenil: Reversing Benzodiazepine Overdose-With Caution
Benzodiazepines like Xanax, Valium, and Klonopin are prescribed for anxiety and sleep. But when mixed with alcohol, opioids, or taken in large doses, they can shut down breathing.Flumazenil is the antidote. It’s given by IV, slowly, in small doses. But here’s the catch: it’s risky. If you’ve been taking benzodiazepines daily for months or years, flumazenil can trigger sudden withdrawal-seizures, panic attacks, even cardiac arrest.
Because of this, many emergency teams avoid flumazenil unless the overdose is clear-cut and the patient has no history of chronic use. Supportive care-oxygen, airway support, monitoring-is often safer. Flumazenil is not a first-line treatment anymore. It’s reserved for rare cases where the overdose is recent, the patient is otherwise healthy, and no other drugs are involved.
If you’re on long-term benzodiazepines, talk to your doctor about overdose risks. Don’t assume you’re safe just because you’re taking it as prescribed. Mixing it with alcohol or opioids is deadly. And if you ever need to be treated for overdose, tell the ER team about your medication history.
Fomepizole: The Antidote for Toxic Alcohols
Ethylene glycol (antifreeze) and methanol (windshield washer fluid) are poison. They taste sweet, so people-especially children or those with mental health struggles-accidentally or intentionally drink them. These substances don’t kill you directly. They turn into acids in your body that destroy your kidneys, eyes, and brain.Fomepizole blocks the enzyme that turns these alcohols into poison. It’s given by IV. The first dose is 15 mg per kg of body weight, then 10 mg every 12 hours. It’s expensive-around $4,000 per treatment-but it works. And it’s safer than the old alternative: ethanol (vodka or whiskey).
Why ethanol? Because alcohol competes with the poison for the same enzyme. It’s a crude, messy workaround. You have to keep giving it, monitor blood levels, and deal with intoxication. Fomepizole is cleaner, more predictable, and doesn’t make the patient drunk. But because of the cost, some rural hospitals still use ethanol as a backup.
If someone drinks antifreeze or windshield fluid-even a sip-get them to the ER immediately. Don’t wait for symptoms. Early treatment with fomepizole can prevent permanent damage.
Methylene Blue: Fixing Methemoglobinemia
Some medications-like certain antibiotics, local anesthetics, or even large doses of nitroglycerin-can turn your blood brown. This condition, called methemoglobinemia, stops oxygen from reaching your tissues. Your lips and skin turn blue-gray. You feel dizzy, short of breath, and confused.Methylene blue is the antidote. It’s given as a slow IV push. The dose is 1 to 2 mg per kg of body weight. It works fast. Within minutes, the color returns to normal. But it’s not for everyone. People with G6PD deficiency (a genetic condition) can have dangerous reactions to methylene blue. That’s why doctors test for it before giving it.
This is rare. But if you’ve been on a new medication and suddenly turn blue, don’t ignore it. Tell your doctor what you’ve taken. Time matters.
What You Can Do Now
You don’t need to be a doctor to save a life. Here’s what you can do today:- Keep naloxone at home if you or someone you live with takes opioids, even for pain. Get it free or for under $25 at most pharmacies.
- Store acetaminophen safely. Keep it locked up if you have kids, teens, or anyone with depression. Never take more than 3,000 mg in 24 hours.
- Know the signs: slow breathing, blue lips, unresponsiveness, confusion, vomiting after taking meds.
- Call 911 first. Then give naloxone if you have it. Don’t wait for EMS to arrive.
- Don’t wait for symptoms. If you suspect an overdose-even if the person seems okay-get help immediately. Liver and kidney damage can be silent until it’s too late.

What Hospitals Can’t Always Tell You
Many people assume hospitals have every antidote on hand. They don’t. Naloxone and NAC are standard. But fomepizole? Only about 38% of rural hospitals keep it stocked. Flumazenil? Often kept only in larger trauma centers.That’s why knowing what to do before you get there matters. If you’re in a rural area, ask your local ER what antidotes they have. If they don’t stock naloxone or NAC, find out where you can get it nearby.
Also, don’t assume insurance will cover everything. NAC IV can cost $700. Fomepizole can hit $4,000. But most plans cover them under emergency care. If you’re worried about cost, tell the ER team. They can often help you find financial aid or patient assistance programs.
Final Reminder: Antidotes Are Not Magic
They’re tools. Powerful ones. But they’re not substitutes for medical care. Naloxone wakes someone up-but they still need to be monitored. NAC saves the liver-but the patient still needs blood tests, fluids, and observation.The best antidote is prevention. Keep meds locked up. Don’t mix alcohol with pills. Don’t take someone else’s medicine. And if you ever think you’ve taken too much-go to the ER. Don’t wait. Don’t hope it’ll pass. Your liver, your lungs, your brain can’t wait.
Can I give naloxone to someone who isn’t overdosing?
Yes. Naloxone only works on opioids. If someone has no opioids in their system, it won’t hurt them. It won’t wake them up if they’re asleep from alcohol or fatigue. But it’s safe to use if you’re unsure. Giving it to someone who doesn’t need it won’t cause harm.
Is it true that NAC tastes awful?
Yes. Oral NAC has a strong, rotten egg smell and bitter taste. Many people gag or vomit it. Hospitals use IV NAC when possible. If you’re given the oral version, ask for it chilled or mixed with juice. Some pharmacies offer flavored versions now. Don’t refuse it because of the taste-it’s saving your liver.
Can I keep flumazenil at home?
No. Flumazenil is not available for home use. It’s only given in hospitals under strict monitoring because of the risk of seizures. If you’re on benzodiazepines long-term, talk to your doctor about a safety plan. Don’t try to get flumazenil on your own.
What should I do if someone overdoses and I don’t have an antidote?
Call 911 immediately. If they’re not breathing, start CPR. If they’re unconscious but breathing, place them on their side in the recovery position. Don’t try to make them vomit. Don’t give them coffee or cold showers. Just keep them safe until help arrives. Emergency responders carry antidotes and can treat them faster than you can.
Are there new antidotes coming soon?
Yes. Researchers are working on longer-lasting versions of naloxone that could last 4 to 6 hours instead of 90 minutes. This would reduce the risk of someone slipping back into overdose. Clinical trials are underway, and some could be available by 2026. But for now, the antidotes we have are proven and effective-if used correctly and in time.
What to Do After an Overdose
Surviving an overdose is just the first step. Many people need follow-up care: addiction treatment, mental health support, medication review. Don’t assume you’re “fine” just because you woke up. Talk to a counselor. Connect with a support group. Overdose is a warning sign-not a one-time event.And if you’ve saved someone’s life with naloxone or by getting them to the ER-you’ve done something extraordinary. Don’t downplay it. You made a difference. Keep learning. Keep being ready.
Comments (15)
-
claire davies December 23, 2025
Okay but can we talk about how wild it is that naloxone is just sitting there in pharmacies like gum or ibuprofen now? I got mine last month because my cousin’s on methadone for chronic pain, and the pharmacist handed it over like it was a coupon for 10% off oat milk. No judgment, no forms, just ‘here ya go, sweetie, save a life.’ I keep it in my purse next to my lip balm. If you’re not carrying it, you’re basically walking around with your eyes closed in a world full of invisible landmines. 🌱
-
Harsh Khandelwal December 25, 2025
lol so now the government’s giving out antidotes like free condoms? next they’ll be handing out oxygen tanks at bus stops. who’s paying for all this? i’m just sayin’-if you’re dumb enough to OD on tylenol, maybe you shouldn’t get a free pass to live. also, why’s everyone acting like fomepizole is some miracle drug? it’s just fancy vodka with a price tag.
-
Lindsey Kidd December 27, 2025
THIS. 🙌 I keep NAC in my medicine cabinet next to my vitamins. My roommate took 5 Advils by accident last year and didn’t tell anyone for 10 hours. We got to the ER at 11. They gave her IV NAC and she was fine. But if we’d waited until she puked? 🤢 I’m telling everyone I know. This isn’t fear-mongering-it’s just common sense. #NACisLife
-
Rachel Cericola December 27, 2025
Let’s be brutally honest: most people don’t know the difference between an overdose and a bad hangover. That’s why public education is non-negotiable. Naloxone isn’t a ‘nice-to-have’-it’s a public health imperative. And NAC? It’s the unsung hero of emergency medicine. If you’re on chronic pain meds, you’re at risk. If you’re a parent, you’re a target. If you’re a friend to someone who’s struggling, you’re their lifeline. Stop treating this like it’s someone else’s problem. Keep naloxone. Know the signs. Act fast. Your silence could cost a life.
-
Blow Job December 28, 2025
Man, I had no idea flumazenil could trigger seizures in long-term users. That’s wild. I’ve got a buddy on Xanax for anxiety and he’s always saying, ‘I’m fine, I just need a little help sleeping.’ But if he ever ODs, the ER docs might not even use the antidote because he’s been on it for years. Scary stuff. I’m gonna tell him to get a medical alert bracelet. No joke.
-
Christine Détraz December 30, 2025
It’s weird how we’ll panic over a broken bone but ignore a silent liver killer. Tylenol is everywhere-cough syrup, cold meds, combo pills. I didn’t even realize I was taking it daily until I checked my meds. Now I write everything down. No more guessing. And yeah, NAC tastes like rotten eggs, but I’d rather gag than end up on a transplant list. 🤢❤️
-
EMMANUEL EMEKAOGBOR January 1, 2026
It is with profound respect for the medical community that I acknowledge the remarkable advancements in antidotal pharmacology. The availability of naloxone in public spaces represents a paradigm shift in emergency response strategy. One must also consider the socioeconomic implications of fomepizole’s cost disparity across rural and urban facilities. Access to life-saving interventions should not be contingent upon geographic location or insurance status. This is not merely medical-it is moral.
-
CHETAN MANDLECHA January 1, 2026
So if I drink antifreeze, I just go to hospital and they give me fomepizole? No jail? No questions? I mean, I get it, save the life, but what about the person who does it on purpose? Is that just… fixed? Like, no consequences? I’m confused.
-
Jillian Angus January 2, 2026
my mom took tylenol for her back and didn’t realize she’d hit the limit for days. she was fine. i didn’t even know about nac until now. i’m gonna print this out and tape it to the fridge. also i keep naloxone in my glovebox. just in case. no big deal
-
Paula Villete January 3, 2026
Wow. So the solution to America’s opioid crisis is… handing out free narcan like candy? And we’re supposed to be impressed? Meanwhile, the real problem-mental health care, poverty, prescription culture-is ignored. Naloxone isn’t prevention, it’s triage. And NAC? Yeah, it works. But why are we letting people accidentally overdose on Tylenol in the first place? Because we treat medicine like cereal. And now we’re surprised when kids eat the whole box? 🤦♀️
-
Georgia Brach January 3, 2026
This article is dangerously oversimplified. Naloxone has been linked to increased opioid use in some studies due to perceived safety. NAC’s efficacy beyond 8 hours is statistically marginal. Flumazenil’s risks are grossly understated. Fomepizole’s cost is a systemic failure, not a triumph. This reads like a pharmaceutical marketing brochure. Where are the caveats? The data? The nuance? This isn’t education-it’s performative optimism.
-
Lu Jelonek January 5, 2026
I work in a rural ER. We don’t have fomepizole. We have ethanol. And yes, we give people vodka IV. It’s messy. It’s old-school. But it works. We’ve saved lives this way for 20 years. I wish we had the fancy stuff. But we don’t. And we still show up. So if you’re in a small town and you hear someone say, ‘We don’t have that drug’-don’t write us off. We’re doing the best we can with what we’ve got.
-
Ademola Madehin January 7, 2026
my cousin OD’d on oxy last year. i gave him narcan. he woke up screaming, ‘why’d you do that?! i wanted to die!’ then he cried for an hour. now he’s in rehab. but i still keep two doses in my wallet. because next time? he might not wake up. and i can’t live with that guilt. this isn’t about politics. it’s about love.
-
Diana Alime January 8, 2026
okay but why is it that if you OD on weed you just chill until it wears off but if you OD on tylenol you’re gonna die? that’s messed up. and why does no one talk about how much of this is just… capitalism? like, why is fomepizole $4000? why isn’t there a generic? why do we need a whole 21-hour IV drip for NAC? someone’s making bank off this. and we’re all just supposed to be grateful?
-
Raja P January 8, 2026
My dad’s on high-dose painkillers after his surgery. I got him a Narcan kit. He laughed and said, ‘I’m not an addict.’ I said, ‘Neither was my cousin. Until she was.’ He didn’t say anything after that. Now he keeps it next to his coffee mug. That’s all it took. Sometimes the bravest thing you can do is just… care enough to act.
