Spastic Muscle: Causes, Treatments, and Practical Management Tips
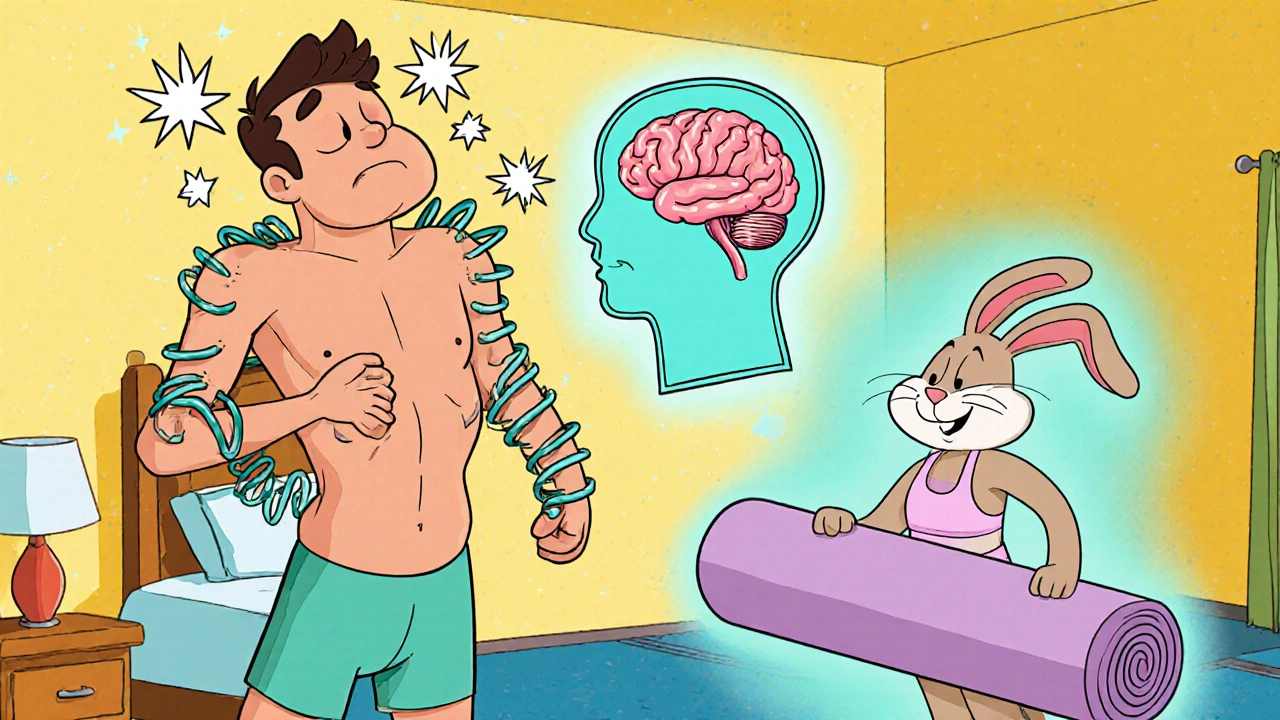
When dealing with spastic muscle, a condition where muscles stay overly tight or constantly contracted, limiting smooth movement. Also known as muscle spasticity, it often shows up after neurological injuries or diseases and can make daily tasks feel like a chore. Understanding its roots helps you choose the right help, whether it’s therapy, medication, or simple home tricks.
One of the biggest triggers of spastic muscle is damage to the brain or spinal cord. Conditions such as cerebral palsy, a group of lifelong disorders affecting movement and posture, stroke, multiple sclerosis, or traumatic brain injury often leave the nerves sending mixed signals that keep muscles in a state of high tone. That high tone, called increased muscle tone, can cause pain, joint deformities, and reduced mobility. Recognizing the link between a specific neurological disorder and the spastic response lets you target treatment more precisely.
Key Approaches to Managing Spastic Muscle
Physical rehabilitation is usually the first line of defense. Physical therapy, a structured program of stretching, strengthening, and functional training works by teaching muscles to relax and lengthen over time. Therapists use techniques like passive stretching, rhythmic stabilization, and task‑specific practice to retrain the nervous system. Adding occupational therapy, focused on fine motor skills and daily‑living activities helps translate those gains into real‑world independence, such as dressing or using utensils.
When therapy alone isn’t enough, doctors may turn to medicines that calm the nerves. Oral baclofen, tizanidine, or diazepam can lower overall tone, but they sometimes cause drowsiness or weakness. For more targeted relief, botulinum toxin, commonly known as Botox, temporarily blocks nerve signals to specific muscles. Injecting Botox into overly tight calves or arms can improve gait, reduce pain, and make stretching easier. Effects last three to six months, so repeat visits are part of the plan.
Supportive devices also play a role. Custom orthotics keep joints aligned while the muscles relax, and serial casting gradually stretches stiff muscles over weeks. In severe cases, surgical options like selective dorsal rhizotomy or tendon lengthening may be considered, but those are usually last‑resort choices after exhaustive conservative care. Regardless of the path you take, a step‑by‑step approach—starting with assessment, followed by therapy, medication, and finally devices—creates a clear roadmap.
Every person with spastic muscle faces a unique mix of challenges, but the tools above are widely available and backed by research. Below you’ll find a collection of articles that dive deeper into each strategy, compare medications, explain how to choose the right orthotic, and give real‑world tips for caring families. Explore the list to find the practical advice that matches your situation and start shaping a smoother, more comfortable daily routine.
Yoga for Spastic Muscle Relief - Benefits, Poses & Safety Tips
Haig Sandavol Oct 15 12Explore how yoga eases spastic muscle states with science‑backed poses, breathing techniques, safety tips, and a simple weekly routine for lasting relief.
More Detail