Pneumothorax Recovery: What Helps, What Hurts, and How Long It Really Takes
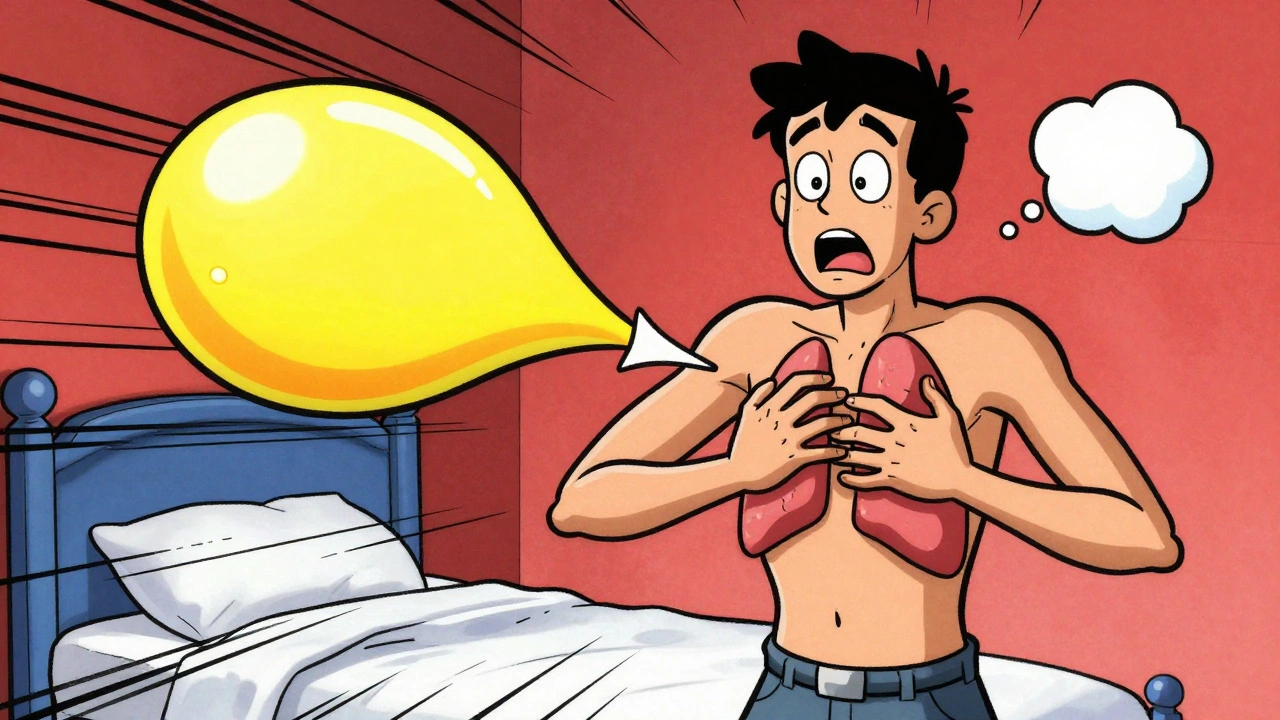
When your pneumothorax, a collapsed lung caused by air leaking into the space between the lung and chest wall. Also known as collapsed lung, it hits, everything stops. You gasp. Your chest tightens. You might not even know why—until the doctor says it’s a pneumothorax. Recovery isn’t just about waiting. It’s about doing the right things at the right time. Some people bounce back in days. Others need weeks. And skipping the basics can mean a second collapse—worse than the first.
What drives recovery? First, the chest tube, a small plastic tube inserted between the ribs to drain air and let the lung re-expand. If your lung is only partly collapsed, you might not need one. But if air keeps leaking, the tube isn’t optional—it’s your lifeline. Then there’s rest. No heavy lifting. No pushing. No coughing hard. Even a strong sneeze can undo progress. Your lung needs space to heal, and your body needs quiet to rebuild the seal. Oxygen helps too. In mild cases, just breathing extra oxygen can speed up air absorption by up to 20%. Simple. Effective. Underused.
And then there’s what slows you down. Smoking? That’s a hard no. Nicotine kills the cells that repair lung tissue. Alcohol? It weakens your immune response and messes with sleep—both critical for healing. Even too much caffeine can raise your heart rate and breathing speed, putting pressure on the healing area. You might feel fine after a week, but the lung’s lining is still fragile. Doctors often warn patients: don’t fly for at least two weeks. Why? Cabin pressure changes can cause trapped air to expand—again—leading to another collapse. And yes, that’s happened. More than once.
Recovery isn’t one-size-fits-all. A young, healthy person with a small spontaneous pneumothorax might be back to walking in 5 days. Someone with trauma, COPD, or a history of lung disease? That’s a different story. It could take 4 to 6 weeks. The key is listening—not just to your body, but to your doctor’s timeline. Skipping follow-up scans? That’s how people end up back in the ER. A simple X-ray after two weeks can show if the lung’s fully expanded or if air’s still hiding.
What you’ll find in these posts isn’t theory. It’s what actually works. From real patient logs on how they managed pain without opioids, to the exact breathing exercises that helped restore lung function, to why some people get recurrent pneumothorax even after surgery. You’ll see how medication safety ties in—even something as simple as avoiding NSAIDs if you’re on blood thinners. You’ll learn how to track symptoms like sudden sharp pain or shortness of breath after activity. And you’ll find out why some people heal faster with physical therapy, while others just need time and patience.
This isn’t about guessing. It’s about knowing what to expect, what to avoid, and when to push—and when to stop. The recovery path is clear if you know the rules. Let’s walk through them.
Pneumothorax: Recognizing Collapsed Lung Symptoms and Getting Emergency Care Fast
Haig Sandavol Dec 2 11A collapsed lung, or pneumothorax, is a medical emergency that requires quick recognition and treatment. Learn the key symptoms, how it's diagnosed, and why immediate care saves lives - plus what to do after you leave the hospital.
More Detail