
More than 1 in 10 adults over 80 in the U.S. take prescription sleep pills every month. That’s not just a number-it’s someone’s mom, dad, or neighbor trying to get through the night. These medications work fast, but they come with hidden costs: memory gaps, next-day fog, falls, and a quiet slide into dependence that many don’t realize is happening until it’s too late.
How Sleep Medications Really Work
Sleep meds don’t help you sleep like a cozy blanket helps you relax. They depress your central nervous system. That means they slow down brain activity so hard that you pass out-sometimes before your body is ready. There are three main types you’ll hear about.Benzodiazepines like lorazepam and diazepam have been around since the 1970s. They boost GABA, a calming brain chemical. But they don’t just target sleep. They affect memory, balance, and coordination. That’s why older adults are warned off them: they increase fall risk by 50-60%.
Z-drugs-zolpidem (Ambien), eszopiclone (Lunesta), zaleplon (Sonata)-were marketed as safer. They hit a narrower target in the brain, so they were thought to cause less next-day grogginess. But that’s not true. The FDA had to lower the starting dose for women in 2019 because so many were waking up with impaired driving skills. One study found residual effects equivalent to a blood alcohol level of 0.05-0.08%. That’s legally impaired in most states.
Off-label drugs like trazodone and doxepin are antidepressants repurposed for sleep. They’re cheaper-sometimes under $10 a month-but carry their own risks. Trazodone can cause priapism (a painful, prolonged erection). Doxepin can mess with heart rhythms at higher doses. And don’t assume OTC options are safer. Diphenhydramine (Benadryl) and doxylamine (Unisom) are antihistamines. Long-term use? A 54% higher risk of dementia, according to JAMA Internal Medicine.
The Dependence Trap
You start with one pill. Then two. Then you forget what life was like without it. That’s not weakness-it’s biology.Benzodiazepines have a 33% dependence rate after just 4-6 weeks of nightly use. Z-drugs are lower, around 5-10%, but still real. The problem isn’t just tolerance. It’s rebound insomnia. When you stop, your sleep gets worse than before. That creates a loop: you feel awful, take the pill again, feel better, and think you need it to survive.
Reddit threads from r/insomnia are full of stories like this: “After six months of Ambien, I quit cold turkey. Couldn’t sleep for three nights. My heart raced. I cried. I went back on it.” That’s not unusual. One JAMA Internal Medicine study found 40% of people trying to quit need extra support-therapy, tapering schedules, or even temporary use of another medication to manage withdrawal.
And it’s not just about sleep. These drugs are Schedule IV controlled substances. That means they’re recognized by the DEA as having abuse potential. Some people crush pills to snort them. Others mix them with alcohol. The NIH says alcohol increases overdose risk by 300%. That’s not a rumor-it’s data.
The Hidden Side Effects
Most people know about drowsiness. Few realize how many other risks are tucked into the fine print.Complex sleep behaviors are terrifying. You’re not dreaming. You’re awake-sort of. You might drive your car, cook a meal, or even have a conversation… and remember nothing. The FDA has logged hundreds of reports of sleep-driving linked to Ambien. Since 2019, the label includes a boxed warning: the strongest kind the FDA can give.
Next-day impairment affects 25% of users. That’s not just feeling tired. It’s slower reaction time, poor decision-making, trouble focusing at work, and memory lapses. One 2022 survey found 27% of users said it hurt their job performance. Imagine being a nurse, a teacher, or a truck driver on this stuff.
And for older adults? The American Geriatrics Society says these drugs are “potentially inappropriate.” Why? Because they increase fracture risk by 20-30%. A single fall can end a person’s independence. Yet, 13% of people over 80 still take them.

What Works Better-And Why
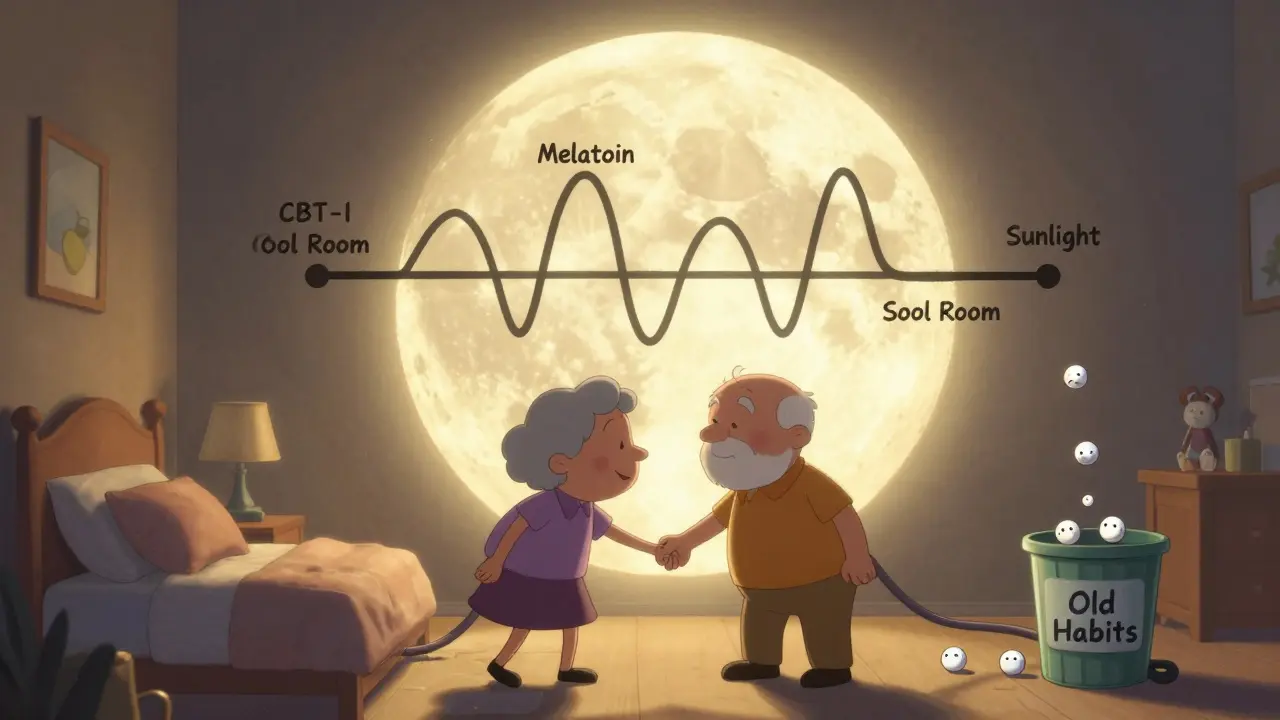
There’s a better way. And it doesn’t come in a bottle.Cognitive Behavioral Therapy for Insomnia (CBT-I) is the gold standard. It’s not just “sleep hygiene.” It’s a structured, evidence-based program that rewires how your brain thinks about sleep. It teaches you to stop lying in bed awake for hours. It breaks the cycle of anxiety around sleep. It helps you rebuild your natural rhythm.
Studies show CBT-I works for 70-80% of people. That’s better than any pill. And the results last. Unlike meds, which lose effectiveness after 4 weeks, CBT-I keeps working months or years later.
It’s not easy. It takes time. Most programs run 6-8 weeks. You’ll keep a sleep diary. You’ll learn stimulus control-only going to bed when sleepy, getting up if you can’t sleep after 20 minutes. You’ll practice relaxation techniques. But 78% of users who tried it say it was more effective long-term than medication, even if the first few weeks felt hard.
Now there’s digital access. The FDA approved Somryst in 2020-a prescription app that delivers CBT-I through your phone. In trials, it helped 60% of users achieve remission. No pills. No side effects. Just a structured program you can do at home.
Other Alternatives Worth Trying
If CBT-I feels too big to start, try these:- Melatonin: A hormone your body makes naturally. Low doses (0.5-3 mg) taken 1-2 hours before bed can help reset your clock. It’s not a sedative. It’s a signal. Reviews on Amazon show high satisfaction-4.2 out of 5-with users praising no grogginess.
- Light exposure: Get 15-30 minutes of natural sunlight in the morning. It tells your brain it’s daytime. That helps you feel sleepy at night.
- Temperature control: Your core body temperature needs to drop to fall asleep. A cool room (65-68°F) helps. A warm bath 90 minutes before bed can trigger that drop.
- Limit screen time: Blue light from phones and TVs blocks melatonin. Try no screens for 60 minutes before bed. Use night mode if you must.
- Exercise: Not right before bed. But 20-30 minutes of moderate activity during the day-walking, cycling, swimming-improves sleep quality over time.
Some people turn to magnesium, valerian root, or chamomile. The science is weaker here. But if they help you relax without side effects? There’s no harm in trying-just don’t expect miracles.
When Medication Might Still Make Sense
I’m not saying all sleep meds are evil. Sometimes, they’re a bridge.If you’re dealing with acute insomnia after a divorce, job loss, or hospital stay, a short course of medication can give you breathing room. That’s okay. But it should come with a plan: “I’ll take this for 2 weeks, then start CBT-I.”
For people with severe depression and insomnia, medication might be necessary alongside therapy. Dr. David Neubauer of Johns Hopkins says: “For some, it’s essential.” But even then, it’s not the goal-it’s the temporary tool.
Doctors should never prescribe these drugs as a first-line treatment. The American Academy of Sleep Medicine says CBT-I should come first. Yet, most prescriptions are written without ever mentioning it.
How to Get Off Sleep Medications Safely
If you’ve been taking these for months or years, don’t quit cold turkey. That’s when rebound hits hardest.Work with your doctor. A safe taper usually means reducing your dose by 25% every two weeks. For example, if you take 10 mg of zolpidem, drop to 7.5 mg for two weeks, then 5 mg, then 2.5 mg, then stop. Some people need even slower.
Use CBT-I during the taper. It helps your brain relearn sleep without the drug. Keep a sleep log. Track your mood, energy, and anxiety. You’ll see patterns. You’ll realize you’re not falling apart-you’re adjusting.
Support matters. Join a group. Talk to others who’ve done it. You’re not alone. And it’s worth it.
What’s Changing in Sleep Medicine
The tide is turning. In 2022, the FDA approved Quviviq (daridorexant), a new type of sleep drug that blocks orexin-a brain chemical that keeps you awake. Unlike Z-drugs, it doesn’t depress your nervous system. Early data shows less next-day drowsiness. It’s promising.Medical schools are starting to teach CBT-I. Hospitals are requiring doctors to refer patients to behavioral therapy before prescribing sleep meds. Insurance companies are demanding proof that you tried non-drug options before covering long-term prescriptions.
The market is shifting, too. Prescription sleep aids made $5.4 billion in 2022. But digital CBT-I apps are growing at 17% a year. Natural supplements are up 9%. The future isn’t more pills. It’s smarter, safer, and more personal.
Can sleep medications cause dementia?
Yes, long-term use of certain sleep aids-especially anticholinergic drugs like diphenhydramine (Benadryl) and doxylamine (Unisom)-is linked to a 54% higher risk of dementia, according to a major study in JAMA Internal Medicine. Benzodiazepines and Z-drugs may also contribute to cognitive decline over time, especially in older adults. The American Geriatrics Society warns against their use in people over 65 for this exact reason.
Is melatonin safer than prescription sleep pills?
Yes, melatonin is generally safer for short-term use. It’s a natural hormone that helps regulate your sleep-wake cycle, not a sedative. It doesn’t cause dependence, next-day grogginess, or complex sleep behaviors. But it’s not a magic fix-it works best for circadian rhythm issues like jet lag or shift work. Doses higher than 3 mg aren’t more effective and can cause headaches or dizziness.
Why do doctors still prescribe sleep meds if they’re risky?
Many doctors are under pressure to solve problems quickly. Patients want relief now. CBT-I takes weeks to show results. A pill works in one night. Also, not all providers are trained in sleep behavior therapy. Insurance often doesn’t cover CBT-I well, making it harder to refer patients. But awareness is growing. More clinics now require behavioral therapy before prescribing long-term meds.
Can I take sleep meds occasionally without getting addicted?
Occasional use-once or twice a week-is lower risk, but not risk-free. Your brain can still adapt. The key is intention. If you’re using them to avoid dealing with stress, anxiety, or poor sleep habits, you’re setting yourself up for dependence. Use them only for true emergencies: a flight across time zones, acute grief, or a short-term medical event. Never make them part of your nightly routine.
What’s the best way to start CBT-I?
Start with a referral from your doctor or a sleep specialist. Look for certified CBT-I providers through the Society of Behavioral Sleep Medicine. If that’s not accessible, try the FDA-approved app Somryst (requires prescription). Many online programs offer self-guided versions. The key is consistency: track your sleep, stick to a schedule, and don’t stay in bed awake. It’s hard at first-but the results last.
If you’re tired of waking up foggy, anxious, or afraid you can’t sleep without a pill, you’re not broken. You’re just caught in a system that favors quick fixes over real healing. The good news? You don’t need another pill. You need a new strategy-and it’s already out there.
Comments (15)
-
Nancy Kou December 20, 2025I used to rely on Ambien for years. Then I tried CBT-I after my doctor finally stopped prescribing it. First two weeks were brutal. I cried. I panicked. But by week six, I was sleeping better than I had in a decade. No pills. No fog. Just quiet, deep rest. It’s not magic-it’s work. And it’s worth every minute.
-
Hussien SLeiman December 21, 2025Let me just say this-every single person who says CBT-I is the answer has never actually tried it while working 60-hour weeks, raising kids, and living in a city where your neighbor plays bass at 2 a.m. The system is broken. Doctors don’t have time. Insurance won’t pay. And the FDA-approved app? It’s a glorified guided meditation with a $200 price tag and a 3-month waitlist. Meanwhile, my 78-year-old dad still gets a script for Lunesta every month because it’s the only thing that lets him sleep through his wife’s snoring. Don’t lecture me about ‘better alternatives’ when the alternatives don’t exist in the real world.
-
Henry Marcus December 22, 2025You think this is about sleep? No. This is about control. The pharmaceutical industry spent billions to convince you that your brain can’t function without a chemical crutch. They pushed benzodiazepines for decades, then Z-drugs, then ‘safe’ antihistamines-each time, same playbook. Now they’re pushing digital apps? Ha! Somryst is just another Trojan horse. The FDA approves it because they’re paid off. The NIH? Owned. The ‘54% higher dementia risk’? Suppressed data. Wake up. The real cure is sunlight, fasting, and quitting sugar. But they don’t want you to know that. They want you addicted. To pills. To apps. To their system.
-
Frank Drewery December 23, 2025I’m a nurse and I’ve seen this firsthand. Elderly patients on sleep meds fall, break hips, end up in rehab-and often never go back home. I’ve had patients cry because they can’t remember their grandkids’ names after months of taking trazodone. I wish more doctors would listen. CBT-I isn’t perfect, but it’s the only thing that actually heals. I’ve referred over 50 people to it. Every single one said they wished they’d started sooner.
-
jessica . December 24, 2025This whole thing is a liberal scam. You want to get rid of pills? Fine. But dont tell me to sit in a dark room and breathe while some app tells me to ‘trust the process’. We used to have discipline. We used to just go to bed. Now we need a $300 phone app and a therapist to tell us not to look at our phones? What happened to America? We used to be tough. Now we’re weak. And the government is helping them sell this nonsense to old people so they can keep their social security checks.
-
Ryan van Leent December 25, 2025I took Ambien for 3 years. Quit cold turkey. Slept 2 hours for 10 days. Felt like I was dying. Went back on it. Now I’m on 5mg. I dont care what you say. It works. I dont want to do some sleep diary. I dont want to meditate. I just want to sleep. If you think I’m weak for taking it then you dont know what real exhaustion is. And no you dont get to judge me for it
-
Sajith Shams December 26, 2025You people are missing the point entirely. The problem isn't the medication. It's the lack of circadian alignment. Your body is not wired for 11 p.m. bedtimes if you're staring at blue light until 1 a.m. and eating carbs at midnight. Melatonin at 0.5mg, 15 minutes of morning sun, and a 68°F room will fix 80% of your ‘insomnia’. No therapy. No apps. Just biology. The rest is placebo and corporate propaganda. I’ve studied chronobiology for 12 years. This is basic science.
-
Ashley Bliss December 27, 2025I used to be the person who took a pill every night because I was terrified of not sleeping. I thought if I didn’t sleep, I’d die. I’d lie there trembling, heart pounding, convinced I’d never close my eyes again. That’s not insomnia. That’s trauma. CBT-I didn’t just teach me how to sleep-it taught me how to stop being afraid of the dark. I cried during my first session. I cried during my last. I’m not fixed. But I’m free. And if you’re reading this and you’re still scared? You’re not alone. I’m here. We’re all here.
-
Elaine Douglass December 28, 2025I tried melatonin and it made me feel like a zombie the next day. I thought it was supposed to be natural and safe. Turns out my body just hates it. I’m sticking with the low-dose zolpidem for now. I know it’s not ideal but I’ve got a big presentation next week and I can’t afford to be a zombie. Maybe next month I’ll try CBT-I. But right now? I need to survive.
-
Takeysha Turnquest December 29, 2025Sleep is the last sacred space we have left. When we outsource it to chemicals, we surrender our souls to the machine. The pills don’t just steal your rest-they steal your dreams. Your memories. Your connection to the quiet rhythm of your own body. We’ve turned the most primal human need into a commodity. And we wonder why we feel so empty. The cure isn’t in a bottle. It’s in silence. In darkness. In stillness. But we’re too afraid to be alone with ourselves anymore.
-
Emily P December 31, 2025Does anyone know if Somryst is covered by Medicare? I’m on a fixed income and I can’t afford $200 for an app. I’ve been on trazodone for 5 years and I want to get off it but I don’t know where to start. Any advice?
-
Jedidiah Massey December 31, 2025The efficacy of CBT-I is statistically significant (p<0.001) with a Cohen’s d of 0.89 in RCTs, per the meta-analysis by Trauer et al. (2015). However, the adherence rate in real-world settings is only 41% due to cognitive load and temporal misalignment with circadian rhythms. Furthermore, the digital delivery model introduces confounding variables related to user interface design and algorithmic bias in sleep stage prediction. We must consider the neurobiological architecture of sleep regulation before advocating for behavioral interventions as panaceas.
-
Lynsey Tyson January 2, 2026I get that some of this sounds overwhelming. But if you’re reading this, you’re already trying. That’s huge. You don’t have to fix everything at once. Maybe just try turning off your phone an hour before bed this week. Or take a warm shower. Or sit outside for five minutes in the morning. Tiny steps. No shame. You’re not broken. You’re just tired. And you deserve rest.
-
Allison Pannabekcer January 4, 2026To anyone feeling alone in this: I started CBT-I at 72. I thought I was too old to change. I was wrong. My therapist was kind. The sleep diary felt silly at first. But after 6 weeks, I slept through the night for the first time in 15 years. I didn’t need a pill. I didn’t need a miracle. I just needed someone to show me how to trust my body again. You can do this. I did.
-
Kitt Eliz January 4, 2026CBT-I is the gold standard-period. 🌟 But let’s be real: access is a nightmare. I’m a sleep coach and I’ve helped 200+ people. Most can’t find a provider within 3 months. That’s why I built a low-cost, sliding-scale group program. We use the same protocols as Somryst but with human support. If you’re struggling, DM me. No judgment. No sales pitch. Just help. You’re not alone. And you don’t need a pill to sleep again.
