Antibiotic-Dairy Timing Calculator
How to Use This Calculator
Enter when you take your antibiotic and when you plan to consume dairy products. The tool will calculate if the timing is safe based on scientific evidence.
Note: This tool focuses on antibiotics most affected by calcium. Always check your specific prescription instructions.
Antibiotic Information
Timing Results
Enter your antibiotic and dairy consumption times to see if your timing is safe.
When you take an antibiotic like doxycycline or ciprofloxacin, your body needs to absorb it properly to kill the infection. But if you swallow that pill right after your morning coffee with milk or a bowl of yogurt, you might be making it much less effective-without even realizing it. This isn’t a myth or old wives’ tale. It’s a well-documented, scientifically proven interaction between calcium in dairy and certain antibiotics. And the timing? It matters more than you think.
How Calcium Stops Antibiotics from Working
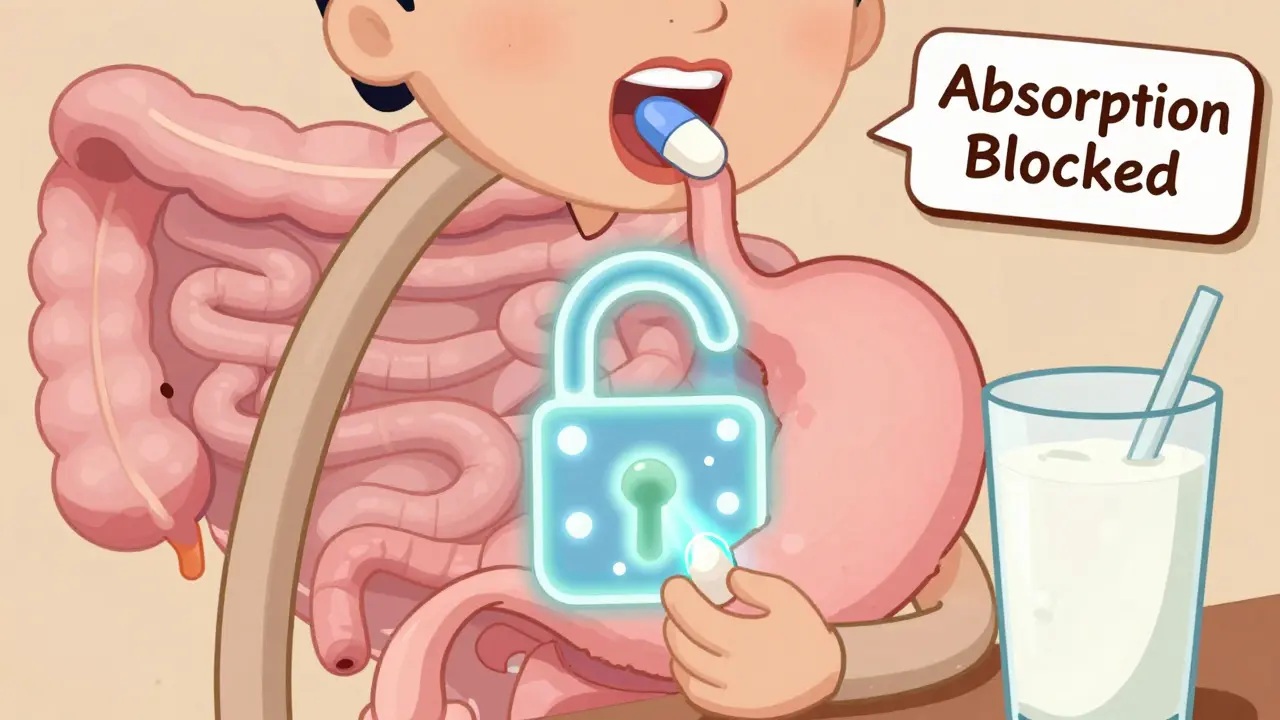
The problem isn’t that dairy is bad for you. It’s that calcium, along with magnesium and iron, binds tightly to specific antibiotics in your stomach and intestines. This binding creates a chemical cage around the drug molecules, turning them into large, insoluble clumps your body can’t absorb. Think of it like putting a lock on the antibiotic so it can’t get into your bloodstream. Once locked up, it just passes through your system and gets flushed out-leaving the infection unchecked.
This chelation process is strongest with two major classes of antibiotics: tetracyclines (like tetracycline, doxycycline, minocycline) and fluoroquinolones (like ciprofloxacin and levofloxacin). Studies show that when these drugs are taken with milk, absorption drops by 20% to over 90%, depending on the antibiotic and how much dairy is consumed. For example, ciprofloxacin with yogurt can lose up to 92% of its absorption. That’s not a small drop-it’s the difference between treatment success and failure.
Which Antibiotics Are Most Affected?
Not all antibiotics react the same way with dairy. Some are barely affected at all. Here’s how the classes stack up:
- Tetracyclines: These are the most sensitive. Tetracycline itself loses 20-75% of its absorption with milk. Doxycycline and minocycline are slightly less affected, but still lose 40-50%. Their chemical structure has specific sites where calcium latches on like a magnet.
- Fluoroquinolones: Ciprofloxacin is hit hard-70-92% reduction with dairy. Levofloxacin is a bit less vulnerable, but still sees a 50-60% drop. These drugs are often used for urinary tract infections, pneumonia, and sinus infections. If you’re taking one, skipping dairy is critical.
- Beta-lactams: Penicillins like amoxicillin and cephalosporins like cefalexin show mixed results. Some studies show a 40% drop in absorption with milk, while others show little to no effect. Amoxicillin, in particular, is generally considered safe with dairy. But if you’re unsure, check your prescription label.
Here’s the bottom line: if your antibiotic is a tetracycline or fluoroquinolone, dairy is a no-go during the critical window. If it’s amoxicillin, azithromycin, or most cephalosporins, you’re probably fine.
How Long Should You Wait?
Timing isn’t just about avoiding dairy at the same time-it’s about giving your body enough space to absorb the drug before calcium shows up.
For tetracyclines, experts recommend taking the antibiotic at least 2 hours before eating dairy-and 4 hours after. That’s because tetracyclines are absorbed quickly in the upper intestine, and calcium sticks to them almost instantly. If you take doxycycline at 7 a.m., you shouldn’t have milk, yogurt, or cheese until after 11 a.m.
Fluoroquinolones need a slightly shorter window: 2 hours before or after dairy. So if you take ciprofloxacin at 8 p.m., wait until 10 p.m. to have your ice cream.
Why the difference? Tetracyclines bind more tightly and form more stable complexes. Fluoroquinolones are a bit more mobile, but still get blocked. The 200 mg calcium threshold is key-about 6 ounces of milk. A single glass of milk or a small cup of yogurt is enough to trigger the interaction. Even a splash in your coffee counts.

What Counts as “Dairy”? (It’s More Than You Think)
When we say “dairy,” we mean anything made from cow’s milk. But the list is longer than most people realize:
- Milk (whole, skim, 2%)
- Yogurt (even sugar-free or probiotic)
- Cheese (hard, soft, shredded)
- Cottage cheese
- Butter and cream
- Ice cream and pudding
- Whey protein powders
- Milk-based coffee creamers
And here’s where people get tripped up: non-dairy doesn’t mean calcium-free. Almond milk, soy milk, oat milk-many of these are fortified with calcium. Some have more calcium than cow’s milk. If your almond milk says “calcium carbonate” or “tricalcium phosphate” on the label, it’s just as dangerous as cow’s milk when taken with antibiotics like doxycycline.
Same goes for antacids (Tums, Maalox), calcium supplements, and iron pills. These all contain minerals that bind to antibiotics. If you take a daily calcium pill at breakfast, don’t take your antibiotic at the same time. Wait 4 hours.
Real-Life Problems Patients Face
Doctors know about this. Pharmacists know about this. But patients? Many don’t.
A 2022 survey of over 1,200 patients found that 63% experienced stomach upset when taking tetracyclines on an empty stomach-so 29% of them just ate dairy anyway to feel better. That’s dangerous. You’re not helping your stomach-you’re sabotaging your treatment.
Reddit threads and pharmacy forums are full of stories. One pharmacist wrote: “I had a patient take doxycycline with a glass of milk and yogurt for breakfast. She came back two weeks later with a worsening rash. Her infection hadn’t cleared because she got only half the dose.”
Another common mistake: taking antibiotics with breakfast, then having milk in coffee at 8:30 a.m. The pill went in at 7 a.m., but the calcium hit the gut at 8:30. That’s too close. Even if you think “I took it an hour before,” it’s not enough.
And then there’s the rhythm problem. Twice-daily dosing makes it hard. If you take your antibiotic at 8 a.m. and 8 p.m., and you eat dairy at lunch and dinner, you’re stuck. You have to choose: skip dairy or adjust your schedule. Most people don’t know how to do this.
What About Newer Antibiotics?
Pharma companies have noticed this problem. Newer formulations are trying to fix it. For example, doxycycline monohydrate (sold as Oracea) is designed to be taken with food-even dairy-without losing effectiveness. The same goes for sarecycline (Seysara), a newer acne treatment that shows only 8% absorption loss with milk.
But here’s the catch: these are exceptions, not the rule. Most antibiotics still follow the old rules. Even if your doctor prescribes a “newer” version, always check the label or ask your pharmacist. Don’t assume.

Why This Matters Beyond Just One Infection
This isn’t just about one missed dose. It’s about the bigger picture.
When antibiotics don’t work because of poor absorption, the infection doesn’t die. It survives. And surviving bacteria? They evolve. They become resistant. That’s how we get superbugs.
The World Health Organization estimates that 1.27 million deaths per year are directly linked to antibiotic resistance. That’s more than malaria or HIV. And a big part of that problem? Incomplete treatment because patients didn’t take their medicine correctly.
Every time you take an antibiotic with dairy and it doesn’t work, you’re not just risking your own health-you’re contributing to a global crisis.
What Should You Do?
Here’s your simple action plan:
- Check your antibiotic class. If it’s doxycycline, minocycline, tetracycline, ciprofloxacin, or levofloxacin, treat dairy as a no-go.
- Read the label. The FDA requires interaction warnings on all affected antibiotics. If it says “take on empty stomach,” avoid dairy for 2-4 hours.
- Time it right. Take the pill 2 hours before or 4 hours after dairy. Set a phone alarm if you need to.
- Watch out for hidden calcium. Check labels on plant-based milks, supplements, and antacids.
- Ask your pharmacist. They have access to databases that flag interactions. Don’t guess.
If you’re taking amoxicillin, azithromycin, or most cephalosporins, you’re likely safe. But if you’re unsure, always double-check. Better safe than sorry.
What If You Already Took Them Together?
Don’t panic. One mistake won’t ruin everything. But don’t repeat it.
If you accidentally took your antibiotic with milk or yogurt, don’t double up on the next dose. That can cause side effects like nausea, dizziness, or even liver stress. Just wait until your next scheduled dose, and make sure to follow the timing rules strictly from then on.
And if you’re on a 7-day course and messed up on day 1? Finish the full course anyway. The infection might be harder to kill now, but stopping early is worse.
Can I drink coffee with milk while taking doxycycline?
No. Even a splash of milk in your coffee can interfere with doxycycline absorption. Wait at least 2 hours after taking the pill before having coffee with milk. Plain black coffee is fine. Same goes for tea with milk or creamer.
Is almond milk safe with antibiotics?
Only if it’s not fortified with calcium. Most almond milk brands add calcium carbonate to mimic cow’s milk. Check the nutrition label. If it lists calcium, treat it like dairy. Use an unfortified version or wait the full 2-4 hours after taking your antibiotic.
Can I eat yogurt while taking antibiotics?
If you’re taking a tetracycline or fluoroquinolone, no. Yogurt has more calcium than milk and often has a lower pH, which makes it even worse for binding antibiotics. Save your yogurt for after your treatment. If you’re on amoxicillin or azithromycin, yogurt is fine and may even help prevent diarrhea.
Why does timing matter more than just avoiding dairy?
Because absorption happens fast. Antibiotics like doxycycline are absorbed in the upper part of the small intestine within 1-2 hours after ingestion. If calcium is present during that window, it binds immediately. Waiting 4 hours ensures the antibiotic is already absorbed and out of the way before dairy enters the system.
What if I have lactose intolerance? Does that help?
Yes, in a way. People with lactose intolerance often avoid dairy naturally, so they’re less likely to interfere with their antibiotic. One study found that lactose-intolerant patients had 18% higher antibiotic absorption rates than those who regularly consumed dairy. But if you still eat yogurt or cheese for the probiotics, you’re still at risk.
Comments (15)
-
Joshua Smith February 8, 2026
I never realized how much calcium could mess with antibiotics. I always took my doxycycline with breakfast and wondered why I kept getting sick. This makes so much sense now. I’ll start timing it right-maybe even switch to black coffee in the morning.
-
Chima Ifeanyi February 8, 2026
Let’s be real-the pharmacopeia is a corporate construct. Calcium chelation? That’s just a convenient narrative to sell more pills. The real issue is bioavailability manipulation by Big Pharma. You think they want you to heal? No, they want you dependent. The ‘2-hour rule’? A myth engineered to keep you coming back.
-
Ritteka Goyal February 10, 2026
OMG this is so true!!! I took cipro with yogurt and got worse, and my cousin in Delhi said the same thing, she had UTI and took amoxicillin with milk and it was fine but then she took cipro and it was disaster!!! So like, in India we don’t really know this, everyone just takes medicine with tea or milk, and now I’m like, wait, is our whole healthcare system broken?? I’m so mad!!
-
Frank Baumann February 12, 2026
Y’all are underestimating how dangerous this is. I had a neighbor take doxycycline with almond milk-‘it’s plant-based, so it’s healthy!’-and ended up in the ER with a raging kidney infection. They had to hospitalize her for 5 days. This isn’t ‘be careful’-this is a silent killer. People think ‘natural’ means safe. Nope. Calcium is calcium. And if you’re not reading labels, you’re gambling with your life.
-
Ken Cooper February 12, 2026
so i just found out my probiotic yogurt has calcium carbonate?? like… what?? i thought it was just for gut health?? i’ve been taking azithromycin with it every day for my sinus infection… oops. i’m gonna switch to plain water for now. also, anyone know if oat milk with added calcium counts? i’m so confused now lol
-
Andrew Jackson February 13, 2026
The erosion of personal responsibility in modern healthcare is alarming. One cannot outsource health to a pill, a label, or a pharmacist. The individual must cultivate discipline. To consume dairy with pharmaceuticals is not merely an oversight-it is a moral failure of self-governance. The West has traded prudence for convenience, and now we suffer the consequences. Discipline, not dosage, is the true cure.
-
Joseph Charles Colin February 15, 2026
For clinical accuracy: the chelation complex formed between divalent cations (Ca²⁺, Mg²⁺, Fe²⁺/³⁺) and tetracyclines/fluoroquinolones has a binding constant in the range of 10⁴–10⁶ M⁻¹, rendering oral bioavailability negligible. The 2–4 hour window isn’t arbitrary-it’s derived from gastric emptying kinetics and intestinal transit time studies. The FDA’s labeling requirements are evidence-based, not advisory. Ignore at your peril.
-
Patrick Jarillon February 15, 2026
Wait… so you’re telling me the government and Big Pharma are hiding the truth? What if the calcium interaction is real… but they *want* you to fail so they can sell you more antibiotics? Think about it. Every time you get reinfected, you get another prescription. It’s a cycle. They even added calcium to almond milk to trick you. This isn’t science-it’s control.
-
Kathryn Lenn February 17, 2026
Oh wow, so I’m not the only one who took my cipro with a latte and then blamed the infection for being ‘stubborn.’ I’m basically a walking antibiotic resistance poster child. Congrats, America. We’ve turned medicine into a guessing game. Also, who decided ‘dairy’ includes creamer? That’s not food, that’s chemical warfare in a carton.
-
Elan Ricarte February 19, 2026
Man, I took my minocycline with a whey shake after the gym. Felt like a hero. Two weeks later? Same damn acne. Now I’m out $80 and a whole lot dumber. This isn’t just about pills-it’s about how we treat our bodies like vending machines. You don’t shove sugar in a diesel engine and expect it to run. Why do it with your gut? Stupid. Dumb. Unforgivable.
-
Angie Datuin February 20, 2026
Thanks for posting this. I’ve been on doxycycline for acne and didn’t know any of this. I just thought I had to take it on an empty stomach. Now I know why my skin kept flaring up. I’ll start timing it right. Really appreciate the clarity.
-
Camille Hall February 21, 2026
This is such an important post. I teach nutrition at a community college, and I’m going to share this with my students. So many young people think ‘plant-based’ means ‘safe with meds’-and they’re not reading labels. We need more awareness. Thanks for breaking it down so clearly.
-
THANGAVEL PARASAKTHI February 23, 2026
in india we drink milk with medicine since childhood, my grandpa used to say 'milk helps medicine go down'… now i know he was wrong. i took cipro with milk last week and my infection got worse. i feel so dumb. i will read labels from now. thanks for this post.
-
Chelsea Deflyss February 24, 2026
sooo… i took my doxycycline with a yogurt parfait and now i’m just supposed to ‘wait’? what if i’m sick and need to feel better? i can’t just live on black coffee and rice for two weeks. this is ridiculous. who designed this system? some lab rat who’s never had a sinus infection?
-
Tricia O'Sullivan February 25, 2026
Thank you for this meticulous and necessary breakdown. I’ve been a pharmacist for 18 years, and I still see patients daily who misunderstand this interaction. Your clarity will help many. Please continue sharing science with compassion.
