Scleroderma is not just a skin condition. It’s a full-body autoimmune disease that causes your body to overproduce collagen, turning soft tissues into hard, tight scar-like material. This isn’t a slow aging process-it’s an immune system gone rogue, attacking your own connective tissues and silently damaging vital organs like your lungs, heart, and digestive tract. Unlike common autoimmune diseases like lupus or rheumatoid arthritis, scleroderma doesn’t just cause swelling or joint pain. It hardens. It tightens. It restricts. And for many, it happens without warning.
What Scleroderma Actually Does to Your Body
Scleroderma, also called systemic sclerosis, has two main forms: localized and systemic. Localized scleroderma only affects the skin-patches of thickened skin on the arms, legs, or torso. It’s rare for this form to spread internally. Systemic scleroderma is the dangerous one. It doesn’t stop at the skin. In 90% of cases, it reaches the gastrointestinal tract, causing severe reflux, difficulty swallowing, and malnutrition. Eighty percent of patients develop lung scarring (pulmonary fibrosis), and 30-45% face heart damage. About 10-15% develop kidney crises that can lead to sudden, life-threatening high blood pressure.
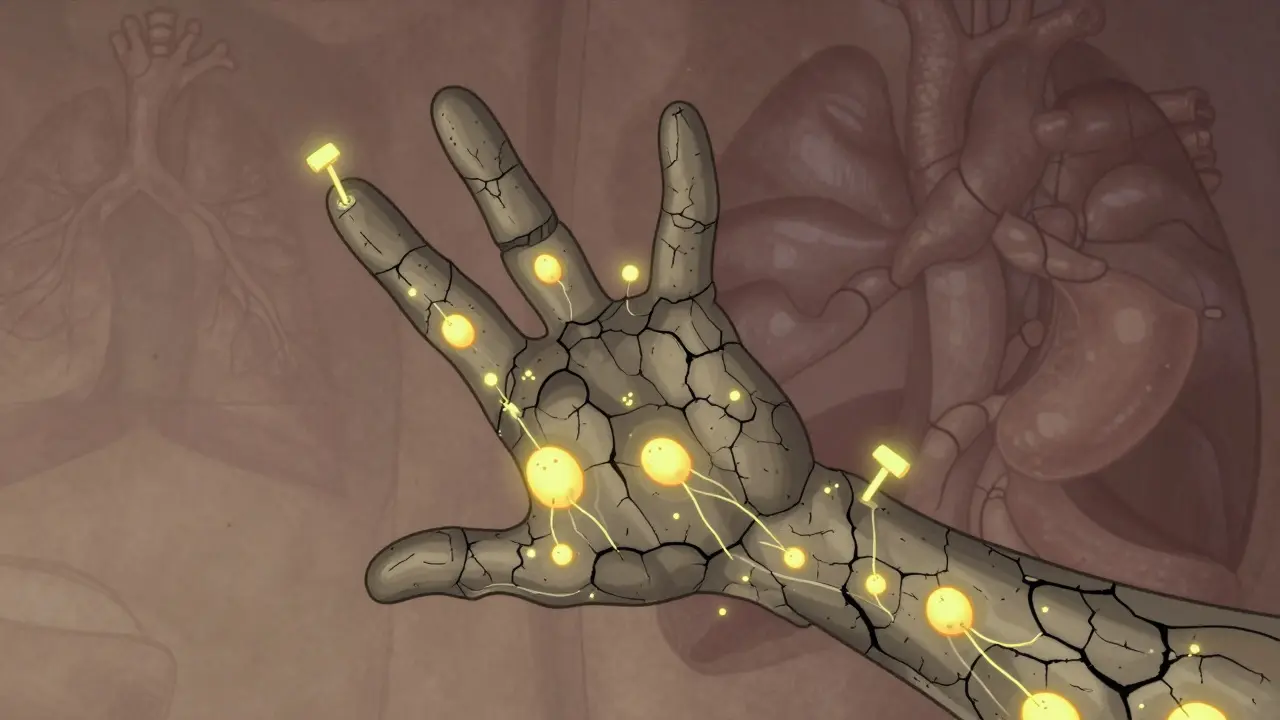
The hallmark sign? Skin that won’t stretch. Fingers become stiff, curled, and hard to move. This isn’t arthritis. It’s fibrosis-the same process that scars a liver after heavy drinking, but happening inside your body from the inside out. The immune system triggers fibroblasts to go wild, making too much collagen. No one knows exactly why. Genetics play a role, but so do environmental triggers like silica dust exposure, certain solvents, or even viral infections. The trigger isn’t the same for everyone, but the result is always the same: tissue that turns rigid.
The Silent Warning Signs Most People Miss
Most patients don’t wake up with scleroderma. They notice something odd months-or years-before a diagnosis. The earliest and most common sign? Raynaud’s phenomenon. When it’s cold, or even when you’re stressed, your fingers turn white, then blue, then red. They feel numb, tingly, or painfully cold. This happens in 90% of systemic scleroderma cases, often 5 to 10 years before other symptoms show up. Many people think it’s just being sensitive to the cold. They don’t connect it to a disease until their fingers start to tighten, or they can’t open a jar anymore.
Then comes sclerodactyly-skin on the fingers thickens so much it pulls the fingers inward. You can’t fully straighten them. Your hands feel like they’re wrapped in plastic wrap. Nailfold capillaries, the tiny blood vessels under your fingernails, become distorted and enlarged. Doctors use a microscope to check these. If they look abnormal, it’s a red flag.
Antinuclear antibodies (ANA) show up in 95% of patients. That doesn’t mean you have lupus-it just means your immune system is activated. But specific antibodies tell doctors what kind of scleroderma you have. Anti-Scl-70 means you’re at higher risk for lung scarring. Anti-centromere antibodies suggest a slower, more limited form. Anti-RNA polymerase III? That’s linked to rapid skin thickening and a higher chance of cancer. These aren’t just lab results. They predict your future.

Why Diagnosis Takes So Long-and Why It Matters
Patients see an average of 3.2 doctors over 18 months before getting the right diagnosis. Why? Because the first symptoms look like other things. Raynaud’s? Common. Fatigue? Everyone gets tired. Acid reflux? Stress or diet. Joint stiffness? Aging. Doctors who haven’t seen a case in years don’t think to test for scleroderma. And even when they do, the tests aren’t always clear.
Early diagnosis changes everything. If you catch lung scarring early, you can start treatments that slow it down. If you monitor blood pressure closely, you can prevent kidney failure. If you treat digital ulcers before they get infected, you avoid amputations. The window to act is narrow-especially in diffuse cutaneous scleroderma, where skin thickening peaks in the first 3-5 years. After that, it may stabilize, but the organ damage is already done.
How Scleroderma Is Different From Other Autoimmune Diseases
Lupus causes flares-periods of intense symptoms followed by calm. Rheumatoid arthritis attacks joints symmetrically, swelling them with inflammation. Polymyositis weakens muscles. Scleroderma? It doesn’t flare. It creeps. It doesn’t swell-it contracts. It doesn’t destroy cartilage-it replaces it with fibrous tissue. That’s why treatments for lupus or RA often don’t work here.
There’s no cure. No FDA-approved drug that reverses fibrosis. Most treatments are borrowed from other diseases: immunosuppressants like mycophenolate, steroids, or blood pressure drugs like ACE inhibitors. Even then, only 40-50% of patients get meaningful relief. A 2023 study found less than 30% of diffuse scleroderma patients improved their skin score after a year of treatment. That’s not failure-it’s the reality of a disease that still lacks targeted therapies.
But things are changing. In 2021, the FDA approved tocilizumab for scleroderma-related lung disease-the first drug ever approved specifically for this. Clinical trials are now testing drugs that block fibrosis pathways, B-cell therapies, and tyrosine kinase inhibitors. The Scleroderma Research Foundation committed $15 million in 2024 to fund these efforts. The future isn’t here yet, but the momentum is growing.
Life With Scleroderma: Daily Struggles and Real Solutions
Imagine not being able to button your shirt. Or holding a coffee cup without dropping it. Or needing to eat six small meals a day because your stomach can’t move food properly. These aren’t hypotheticals. In a 2023 survey of 1,245 patients, 78% said hand contractures made daily tasks impossible. 65% needed adaptive tools. 82% had severe GI issues. 70% were too tired to work full-time.
Managing this isn’t about one pill. It’s about a whole team. A rheumatologist who specializes in scleroderma. A pulmonologist to monitor lung function with yearly CT scans and breathing tests. A cardiologist to check for pulmonary hypertension with echocardiograms. A gastroenterologist to handle reflux and motility problems. A wound care specialist for digital ulcers. A physical therapist to maintain mobility.
Patients who see a multidisciplinary team at centers like Johns Hopkins, Stanford, or the University of Michigan report 68% better symptom control than those treated by general rheumatologists. Telemedicine programs are helping reach rural patients-Stanford’s program cut hospitalizations by 32% in its first six months.
What’s Next for Scleroderma Patients?
The biggest shift isn’t just in treatment-it’s in survival. Ten-year survival rates for limited scleroderma are now 75-85%. For diffuse, they’re 55-70%. That’s better than it was 20 years ago. But as people live longer, new problems emerge. Many patients over 65 now face scleroderma alongside diabetes, heart disease, or osteoporosis. Managing all of them together is complex.
Research is moving fast. Autologous stem cell transplants showed 50% improvement in skin thickness after 4.5 years in the 2023 SCOT trial. New blood biomarkers like CXCL4 could detect scleroderma before symptoms appear. That’s the holy grail: prevention, not just management.
But access remains a problem. Only 35% of U.S. patients see a scleroderma center of excellence. Many live hours from the nearest specialist. Insurance often denies expensive treatments like iloprost infusions, even when they’re life-saving. Advocacy groups are pushing for better coverage and more research funding.
Scleroderma doesn’t make headlines. It doesn’t have celebrity fundraisers. But for 300,000 Americans and nearly a million people worldwide, it’s the quiet storm inside their bodies. It doesn’t go away. But with better diagnosis, better care, and better science, it doesn’t have to define your life.
Comments (14)
-
Dan Alatepe December 26, 2025This hit me like a truck. I’ve had Raynaud’s since I was 16 and thought it was just ‘being dramatic’ 😅 Now I’m scared to check my nailfold capillaries. If this is the silent storm… I didn’t even know I was in the hurricane.
-
Angela Spagnolo December 27, 2025i just read this... and... wow. i didn't know scleroderma could do *that* to your insides. i thought it was just... tight skin. like, really tight. but lungs? heart? digestive system? oh my god. i'm so sorry to everyone living this.
please, if you're reading this and have weird finger changes... get checked. don't wait.
-
SHAKTI BHARDWAJ December 28, 2025LMAO so now we’re giving autoimmune diseases poetry readings? ‘It doesn’t flare-it creeps.’ Cute. Sounds like someone wrote this for a TED talk. Where’s the real data? 30% improvement? That’s not treatment, that’s a placebo with a fancy name. And who funded this? Pharma? 😒
-
Matthew Ingersoll December 29, 2025In Nigeria, we don’t have access to rheumatologists, let alone scleroderma specialists. I’ve seen women with hand contractures working in markets, unable to hold their goods. No scans. No ACE inhibitors. Just prayers and herbal tea. This isn’t just a medical issue-it’s a global justice issue.
-
carissa projo December 29, 2025I want to sit with everyone who just read this and say: you are not alone. The fatigue? The inability to hold a cup? The fear that your body is turning against you? It’s real. And it’s valid. You don’t have to be ‘strong’ to survive this-you just have to keep breathing.
There’s a whole community out there-online, in support groups, in quiet corners of hospitals-holding space for you. Even if no one else sees it, we see you.
-
josue robert figueroa salazar December 31, 2025No cure. 40% response rate. Kidney crises. Lung scarring. Hand amputations. And they call this medicine? We’re just managing decline. They’re not curing. They’re delaying. And calling it progress.
-
david jackson January 1, 2026I’ve been reading about fibrosis for weeks now and it’s terrifying how similar this is to liver cirrhosis-but happening internally, silently, without alcohol, without warning. It’s like your body is trying to heal itself… but the healing process goes rogue and turns your organs into concrete.
And the worst part? The antibodies predict your future like a horoscope. Anti-Scl-70? You’re gonna lose lung function. Anti-centromere? Maybe you’ll live longer but never hold your grandkid’s hand properly. It’s not just a disease-it’s a sentence.
-
Jody Kennedy January 2, 2026To anyone reading this who feels hopeless: there IS progress. Tocilizumab was approved in 2021. Stem cell trials are showing real results. CXCL4 biomarkers might let us catch this before symptoms start. You’re not waiting for a miracle-you’re waiting for science to catch up. And it’s running faster than you think.
-
jesse chen January 3, 2026I just shared this with my rheumatologist. She said she’s seen maybe 3 cases in 15 years. That’s not rare-that’s a system failure. We need more training. More awareness. More funding. This isn’t a niche disease. It’s a silent epidemic that no one talks about because it doesn’t look like cancer or MS. But it kills just the same.
-
Joanne Smith January 3, 2026Oh sweetie, you really think the FDA approved tocilizumab because they care? Nah. It was repurposed from RA. They didn’t invent anything-they just recycled a drug and slapped a new label on it. ‘First drug approved for scleroderma lung disease’ sounds heroic. It’s just corporate branding with a side of hope.
-
Prasanthi Kontemukkala January 4, 2026I’m from India and my cousin has limited scleroderma. She can’t button her clothes, but she still teaches yoga to kids. She says, ‘My hands may be stiff, but my spirit isn’t.’ I don’t know if science will fix her body-but her courage? That’s the real breakthrough.
-
Alex Ragen January 4, 2026The romanticization of suffering is exhausting. ‘Quiet storm inside their bodies’? Poetic. But what’s the cost? The $20,000 infusions? The lost jobs? The insurance denials? This isn’t a metaphor-it’s a financial and physical burden. And yet we celebrate ‘resilience’ instead of demanding systemic change. How noble.
-
Lori Anne Franklin January 5, 2026i just found out my aunt has this and she never told anyone. she just said her hands were ‘getting old’. now i’m crying. i’m gonna send her this article. she needs to know she’s not crazy. and she’s not alone.
-
Bryan Woods January 6, 2026The data presented is methodologically sound. The prevalence figures, survival rates, and treatment response metrics align with peer-reviewed literature from the Journal of Rheumatology and Arthritis & Rheumatology. The multidisciplinary care model is supported by Level 1 evidence. This is one of the most accurately reported patient narratives on systemic sclerosis I’ve encountered in a public forum.
