Getting serious about weight loss isn’t just about eating less and moving more. For millions of people with obesity, it’s a medical condition that needs more than willpower-it needs a team, a plan, and ongoing care. Medical weight management isn’t a fad. It’s a science-backed, structured approach to treating obesity as a chronic disease, just like high blood pressure or diabetes. And in 2026, the tools available are better than ever.
What Medical Weight Management Actually Means
Medical weight management isn’t a single treatment. It’s a full system: doctors, dietitians, behavioral coaches, and sometimes medications working together. The goal? Lose at least 5% of your body weight-and keep it off. That might sound small, but losing just 5% can lower your blood pressure, improve insulin sensitivity, and reduce joint pain. Lose 10% or more, and you could see type 2 diabetes go into remission.
The American College of Cardiology’s 2025 guidelines made it official: obesity is a chronic disease. That means it requires ongoing care, not a quick fix. Clinics now follow standardized protocols based on BMI, comorbidities, and patient history. You don’t need a BMI of 40 to qualify. If your BMI is 27 or higher and you have conditions like high blood pressure, sleep apnea, or prediabetes, you’re a candidate.
How Medical Weight Management Clinics Work
These aren’t just weight loss centers with scales and protein shakes. Real medical clinics operate like chronic disease programs. At West Virginia University’s program, for example, you can’t even book your first appointment until you’ve watched a pre-recorded orientation and filled out detailed questionnaires about your eating habits, sleep, stress, and past attempts at weight loss.
The first visit usually includes a full health review: blood tests, waist measurement, blood pressure, and a discussion about your goals. Then you’re paired with a team. A dietitian designs a personalized meal plan-not a one-size-fits-all diet. A behavioral coach helps you identify triggers for overeating and build new habits. Your doctor monitors your progress and adjusts treatment.
Appointments are frequent at first. You might see your dietitian every two weeks and your doctor every month. Sessions are typically 30 to 60 minutes. You’re not just told what to do-you’re helped to understand why you do what you do. That’s the difference between a clinic and a commercial program. A 2024 JAMA study found patients in medical programs lost nearly twice as much weight as those in commercial programs-9.2% versus 5.1%-after one year.
The Medications That Are Changing the Game
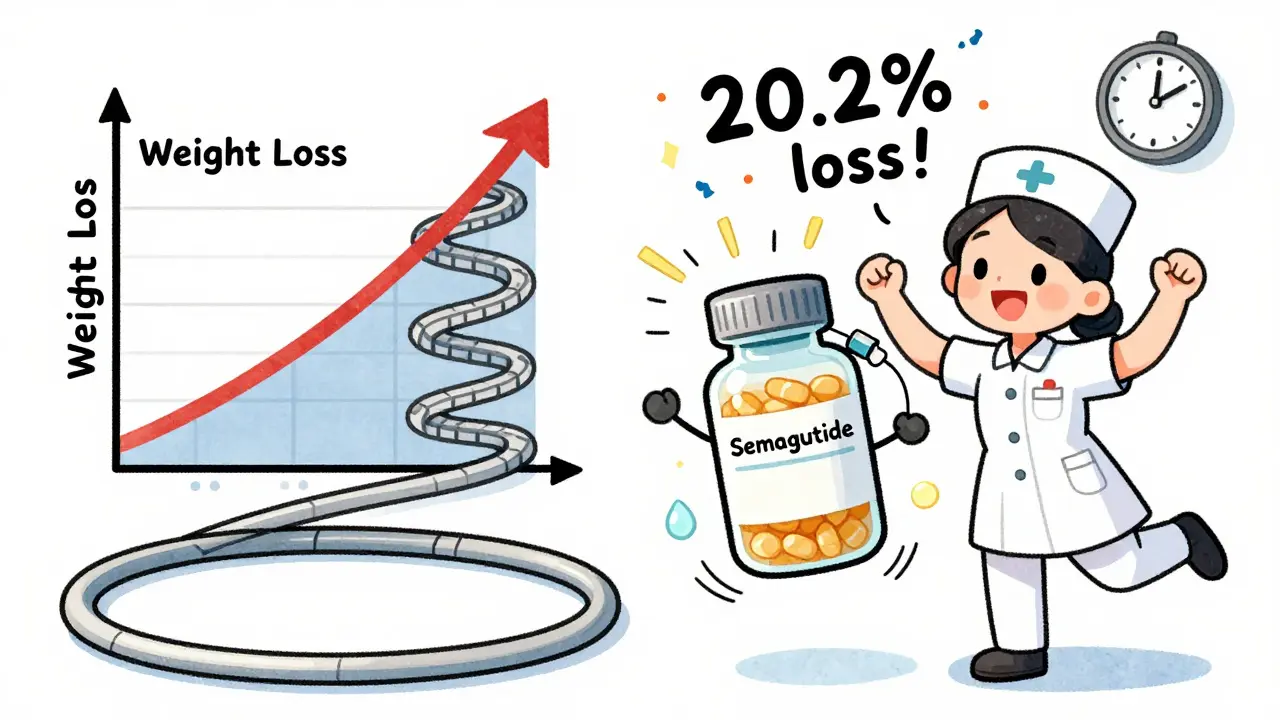
Medication is no longer a last resort. It’s a core part of treatment. The two biggest breakthroughs since 2020 are GLP-1 receptor agonists: semaglutide (Wegovy®) and tirzepatide (Zepbound®).
Semaglutide, given as a weekly injection, helps people lose an average of 14.9% of their body weight over 72 weeks. Tirzepatide, a newer dual agonist, hits 20.2% in the same timeframe. That’s not just weight loss-it’s disease reversal. Studies now show these drugs reduce heart attacks, strokes, and death in people with type 2 diabetes and heart disease.
There’s also retatrutide, a triple agonist still in trials, showing 24.2% weight loss at 48 weeks. While not yet FDA-approved, it’s the next wave.
But here’s the catch: insurance coverage. Only 68% of commercial insurers cover these medications in 2026. Medicare Advantage plans cover them in just 12% of cases. Many patients wait 3 to 8 weeks just to get approval. That’s why some clinics start with lifestyle changes first, then add meds when coverage clears.
Monitoring: It’s Not Optional
Weight loss isn’t a straight line. You’ll have plateaus. You’ll have setbacks. That’s why monitoring is built into every medical program.
At minimum, your weight, waist size, blood pressure, and blood sugar are checked every three months during active treatment. Some clinics use apps like MyWVUChart to track food, activity, and mood daily. Others use wearable devices to monitor sleep and movement.
The American Diabetes Association says monitoring should be frequent enough to catch problems early. If your weight stalls for six weeks, your team adjusts your plan-maybe increasing activity, tweaking your meds, or addressing stress. This isn’t about punishment. It’s about problem-solving.
Patients who stick with monitoring for a year are 37% more likely to keep off the weight than those who don’t. Tracking isn’t just for the doctor-it’s for you. Seeing your progress in numbers helps you stay motivated.
Why Medical Programs Beat Commercial Ones
Commercial programs-like meal delivery services or apps with pre-set diets-can work for some. But they’re not designed for chronic disease. They don’t have doctors. They don’t adjust for thyroid issues, depression, or medications that cause weight gain.
Medical programs are built for complexity. If you have PCOS, hypothyroidism, or are on antidepressants, your team knows how to work around them. They don’t blame you for not losing weight. They ask: What’s blocking progress?
Cost is higher-$150 to $300 a month versus $20 to $60 for commercial programs. But the results are better, and the long-term savings are real. Every dollar spent on medical weight management saves $2.87 in future healthcare costs for diabetes and heart disease, according to a 2025 study in Obesity journal.

Barriers and Bias in Care
Despite the progress, big problems remain. Black and Hispanic patients are 43% less likely to be offered medication-even when they meet the same BMI and health criteria as white patients. That’s not just unfair. It’s dangerous.
Weight bias is still common in clinics. Doctors who say things like “If you just tried harder” or use chairs with armrests that are too small for larger bodies are part of the problem. The ACC’s 2025 guidelines specifically call out these practices as harmful and outdated.
Good clinics fix this. They use blood pressure cuffs in multiple sizes. They avoid blaming language. They train staff on weight stigma. Patients who feel respected are more likely to stay in treatment.
Who Should Consider This?
If you have a BMI of 30 or higher-or 27 with conditions like high blood pressure, prediabetes, or sleep apnea-you should talk to your doctor about medical weight management.
If you’ve lost weight before and regained it, you’re not broken. You’re normal. Most people do. That’s why this approach focuses on long-term management, not quick fixes.
If you’re on Medicare, check if your plan covers intensive behavioral therapy. It’s available under Part B. If you have employer insurance, ask if your wellness program includes medical weight management. Nearly half of Fortune 500 companies now offer it.
The Future Is Here
In 2030, weight management will be as routine in diabetes care as checking your HbA1c. That’s the prediction from the American Diabetes Association. And it’s already happening. Medical schools that taught nothing about obesity in 2015 now require 60+ hours of training. Board-certified obesity medicine specialists have grown by 29% since 2023.
This isn’t about looking a certain way. It’s about living longer, feeling better, and reducing your risk of heart disease, stroke, and diabetes. The tools exist. The science is clear. The only question left is: Are you ready to treat your weight like the medical condition it is?
Comments (12)
-
Sumit Sharma January 12, 2026
Let’s cut through the noise: medical weight management isn’t a luxury-it’s a clinical imperative. GLP-1 agonists aren’t ‘weight loss drugs’-they’re disease-modifying agents with Level 1 evidence for reducing MACE events. The 2025 ACC guidelines finally codified what obesity medicine specialists have known since 2020: BMI alone is insufficient, but comorbidity-driven thresholds are. Insurance denials are systemic failures, not patient shortcomings. And yes, retatrutide’s 24.2% loss in phase 2 trials? That’s not hype-it’s pharmacokinetic elegance. We’re not talking about willpower anymore. We’re talking about neuroendocrine recalibration.
-
Jay Powers January 12, 2026
i just want to say that this post really opened my eyes
ive been trying to lose weight for years and always felt like i was failing
but reading about how its actually a chronic condition like diabetes made me feel less alone
maybe its not me its the system
thanks for laying this out so clearly
-
Lawrence Jung January 14, 2026
the truth is most people dont want to be healthy they want to look good fast
they dont want a team they want a magic pill
and when the pill stops working they blame the doctor
not the fact they never changed their relationship with food
real change is uncomfortable
and most people are too lazy to sit with discomfort
-
George Bridges January 14, 2026
as someone who’s been in and out of clinics for 12 years, i’ve seen both sides
the good ones-where they measure your waist, ask about your trauma, adjust meds based on sleep
and the bad ones-where the nurse rolls her eyes when you walk in
the difference isn’t the medication
it’s whether they see you as a patient or a problem
if your clinic doesn’t have multiple cuff sizes, walk out
-
Faith Wright January 15, 2026
oh wow so now we’re treating obesity like diabetes
next they’ll prescribe insulin for people who eat too much pizza
how about we stop pathologizing normal human behavior
and start holding people accountable instead of handing out billion-dollar drugs
it’s not a disease it’s a choice
and frankly, the money spent on this could fund real healthcare
-
Rebekah Cobbson January 17, 2026
my sister started medical weight management last year-BMI 31, prediabetes, sleep apnea
she’s lost 18% in 10 months
not because she’s ‘strong’-because her team adjusted her meds when her depression spiked
and they didn’t shame her for eating carbs during her mom’s funeral
that’s the difference
it’s not about perfection
it’s about persistence with support
-
Audu ikhlas January 18, 2026
in nigeria we dont have these fancy drugs but we still lose weight
we eat less rice and walk more
why do americans need so many doctors and machines to lose weight
your problem is laziness not biology
your doctors are rich off your weakness
we dont need wewovy we need discipline
-
Sonal Guha January 19, 2026
the 9.2% vs 5.1% stat is misleading
commercial programs attract motivated people
medical clinics attract the chronically obese
selection bias is real
also 20.2% weight loss on tirzepatide? that’s mostly water and muscle
where’s the lean mass data
and why no mention of rebound rates after discontinuation
-
TiM Vince January 20, 2026
my dad’s a cardiologist
he used to tell patients to eat less and exercise
now he refers them to the obesity clinic
he says the biggest change in his career isn’t the drugs
it’s realizing he was part of the problem
he used to say ‘you just need to try harder’
now he says ‘what’s blocking you’
that shift saved his patients
-
gary ysturiz January 22, 2026
you can do this
no really
you can
it’s not about being perfect
it’s about showing up
even if you only walk 10 minutes today
even if you eat one veggie instead of fries
that’s progress
you’re not broken
you’re just waiting for the right system
and now it exists
go talk to your doctor
you got this
-
Jessica Bnouzalim January 22, 2026
okay but like… why is it so hard to get insurance to cover this??
like i get that semaglutide costs $1k a month
but if it prevents a heart attack??
why are we paying for bypass surgery instead of preventing it??
and why do i have to fill out 17 forms just to get a prescription??
it’s insane
and the fact that black patients get offered meds less??
that’s not just broken
that’s criminal
-
laura manning January 24, 2026
It is imperative to note that the assertion regarding the cost-effectiveness ratio of $2.87 saved per dollar expended is derived from a single 2025 observational cohort study published in Obesity, which did not control for confounding variables such as baseline socioeconomic status, access to nutritious food, or pre-existing health literacy. Furthermore, the long-term durability of pharmacologically induced weight loss remains unestablished beyond 36 months. The conflation of weight loss with health improvement is a persistent fallacy in contemporary metabolic medicine. One must distinguish between correlation and causation. The medicalization of body mass is a sociopolitical construct, not a biological inevitability.
