
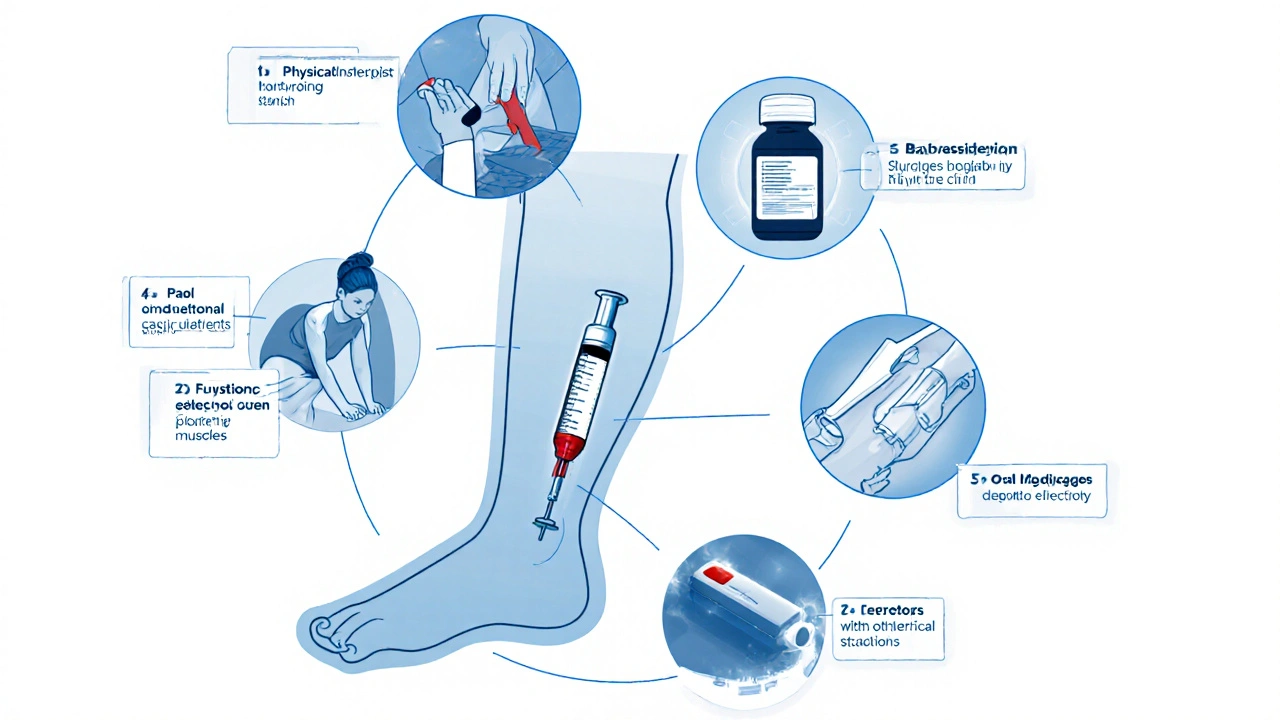
Spasticity Treatment Selector
Recommended Treatments
Physical Therapy
Improves range of motion and function. Starts early, typically around 2 years.
Botox Injections
Targets specific muscles. Usually starts around 4 years old.
Oral Medications
Systemic approach. Often used alongside other treatments.
When a child’s muscles stay tight or jumpy for no clear reason, daily life can feel like an obstacle course. Spastic muscle states are a group of conditions where muscle tone is abnormally high, limiting smooth movement and causing pain, fatigue, or joint problems. Understanding why this happens, spotting the warning signs early, and choosing the right mix of therapies can turn a frustrating routine into a manageable one.
Quick Takeaways
- Spasticity is most often linked to neurological conditions like cerebral palsy, but it can also appear after injury or infection.
- Early assessment by a pediatric neurologist or physical therapist improves long‑term outcomes.
- Combining stretching, targeted therapy, and, when needed, medical interventions (Botox, oral meds, surgery) gives the best functional gains.
- Home‑based routines are essential; consistency beats occasional intensive sessions.
- Support networks-parent groups, school therapists, and insurance counselors-can remove many hidden barriers.
What Exactly Is a Spastic Muscle State?
In simple terms, a spastic muscle stays partially contracted even when you’re not trying to move it. The nervous system sends too much signal, leading to "hypertonia"-excessive muscle tone. This differs from "rigidity," which is a uniform resistance felt in conditions like Parkinson’s. Spasticity is velocity‑dependent: the faster a limb is moved, the more resistance you feel.
Common Causes in Kids
Most children with spasticity have an underlying neurological diagnosis. The most frequent are:
- Cerebral palsy - a static brain injury occurring before, during, or shortly after birth.
- Traumatic brain injury - severe blows to the head during early childhood.
- Stroke - rare in kids but possible in neonatal periods.
- Genetic disorders like hereditary spastic paraplegia.
Even a mild concussion can trigger temporary spasticity, so keep an eye on any head trauma, no matter how small.
Spotting the Signs Early
Parents are the first clinicians. Look for these red flags:
- Limbs feel stiff or “tight” especially after a nap.
- Unexplained crawling or walking on toes.
- Frequent tripping, even on flat surfaces.
- Difficulty with fine motor tasks - buttoning, writing, or using utensils.
- Visible muscle bulk (sometimes called “spastic calves”).
If two or more appear consistently, schedule a evaluation with a pediatric neurologist or a certified pediatric physical therapist.
Choosing the Right Treatment Mix
No single approach fixes spasticity for everyone. The most effective plans blend several modalities, each targeting a specific goal.
| Treatment | Primary Goal | Invasiveness | Typical Age Start | Duration of Effect |
|---|---|---|---|---|
| Physical therapy | Improve range of motion, strength, and functional skills | Non‑invasive | 2years+ | Continuous - benefits maintain with regular sessions |
| Botulinum toxin (Botox) | Temporarily relax overactive muscles | Minimally invasive (injection) | 4years+ | 3-6months per cycle |
| Oral antispastic drugs (e.g., baclofen) | Systemic reduction of tone | Non‑invasive (pill) | 5years+ | While medication is taken; side‑effects may limit use |
| Orthopedic surgery | Correct contractures, improve alignment | Highly invasive | 6-12years (depending on growth plates) | Long‑term, but may need repeat procedures |
| Functional Electrical Stimulation (FES) | Activate weakened muscles while reducing spastic overactivity | Non‑invasive (surface electrodes) | 7years+ | Effect lasts during stimulation; benefits grow with training |
Most clinicians start with physical therapy, add Botox for focal spikes, and consider oral meds only when tone is widespread. Surgery is a last resort, usually after growth‑related contractures become rigid.
Home‑Based Strategies That Really Work
Even the best clinic plan stalls without daily practice at home. Here are three proven habits:
- Daily Stretch Routine - Spend 10minutes each morning gently pulling the tight muscle into a comfortable length. Use a 30‑second hold, repeat 3-5 times. Stretching improves connective tissue elasticity and reduces sudden “catch” episodes.
- Task‑Specific Practice - Instead of generic exercises, rehearse the exact skill the child needs (e.g., brushing teeth, opening a jar). Repetition builds neural pathways that override spastic signals.
- Positioning and Orthotics - Night splints or daytime ankle‑foot orthoses keep joints in a neutral position, preventing contracture formation.
Consistency beats intensity: a short, daily session is more beneficial than a long, sporadic one.

When to Call in the Professionals
If you notice any of the following, it’s time to schedule a specialist visit:
- Rapid increase in tone that interferes with feeding or breathing.
- New pain, swelling, or skin breakdown around a tight joint.
- Loss of previously achieved milestones (e.g., a child who could stand now falls frequently).
- Difficulty fitting shoes or clothing due to muscle bulk.
Early intervention can prevent secondary complications like scoliosis or hip dislocation, which become harder to treat later.
Resources, Support, and Next Steps
Managing spasticity isn’t a solo mission. Tap into these community assets:
- Parent Groups - Organizations like United Cerebral Palsy host local meet‑ups and online forums.
- School Therapy Services - Many districts provide physical and occupational therapy at no extra cost.
- Insurance Navigation - A dedicated case manager can streamline approvals for Botox, orthotics, or surgical consultations.
- Research Registries - Enrolling in a clinical trial gives access to cutting‑edge treatments and expert oversight.
Start by creating a simple log: date, activity, observed tone level (low/medium/high), and any pain notes. Share this with your therapist at each visit - it speeds up treatment adjustments and shows progress over time.
Frequently Asked Questions
Can spasticity improve on its own as a child grows?
In some cases, especially after a mild brain injury, muscle tone normalizes as the nervous system matures. However, most children with cerebral palsy or long‑standing conditions retain some degree of spasticity throughout life, making therapy essential.
Is Botox safe for kids under five?
Botulinum toxin has been approved for pediatric use in many countries for children as young as two when administered by an experienced neurologist or orthopedic surgeon. The doses are weight‑based, and side‑effects are usually mild (temporary weakness, bruising).
How often should my child see a physical therapist?
For moderate spasticity, 2‑3 sessions per week are typical in the first six months, tapering to weekly or bi‑weekly maintenance once goals are met. The exact frequency depends on the child’s motivation, home practice adherence, and the therapist’s assessment.
What are the signs that surgery might be needed?
When a joint becomes permanently stiff (contracture), causing pain or functional loss, and conservative measures fail after 12‑18months, orthopedic surgeons consider procedures such as tendon lengthening, osteotomies, or selective dorsal rhizotomies.
Can oral medications replace therapy?
Oral drugs can lower overall tone but rarely restore functional skills. They are most useful as an adjunct to therapy, especially when spasticity is diffuse and interferes with sleep or comfort.
Comments (19)
-
Shanmughasundhar Sengeni October 8, 2025
Spasticity treatment shouldn't be a one‑size‑fits‑all billboard. The nuances between focal Botox injections and whole‑body oral meds are huge. Kids aren't just little adults, their neuromuscular systems develop at different paces. Early PT lays the groundwork, but you still need to watch for contracture signs. If you ignore the timing, you risk more invasive surgery later.
-
ankush kumar October 9, 2025
Okay, so imagine you have a kid who's just learning to walk and suddenly their calf feels like a steel rope. First thing you want: gentle, consistent stretching – not some marathon session that leaves them exhausted. I always tell parents to set a timer for 30 seconds, repeat three to five times, and actually write it down in a log so they don’t forget.
Then, integrate the stretch into daily routines – like right after brushing teeth or before bedtime.
Task‑specific practice is another gem: if they struggle with buttoning, have them practice that exact motion over and over, not just generic arm waves.
And don’t forget orthotics; a well‑fitted night splint can save months of therapy down the line.
Consistency beats intensity any day, so keep it short, keep it daily, and celebrate the tiny wins.
-
Cameron White October 9, 2025
Look, the pharma industry loves to push pills for everything. Spasticity is a neurological issue, not a chemical fix. Keep an eye on real‑world outcomes, not just what the ads say.
-
Amélie Robillard October 10, 2025
Totally get the frustration – it's like trying to untangle earbuds in the dark. 😅 Keep the kids moving with fun games, and remember: a little progress is still progress. 🎉
-
Fae Wings October 10, 2025
Seeing a child battle spasticity feels like watching a silent storm – the tension builds, the effort is invisible, yet the outcome is dramatic. When a simple stretch eases that tension, it's a mini‑miracle worth celebrating. Don't let the daily grind dull that feeling. Your support can turn a bleak moment into a hopeful one.
-
Anupama Pasricha October 11, 2025
From a biomechanical perspective, integrating neuromuscular facilitation with orthotic management can modulate gamma‑motor drive, reducing hypertonic bursts. Ensure the AFO is calibrated for neutral dorsiflexion to prevent maladaptive contracture formation. Monitoring EMG feedback during PT sessions can also fine‑tune the dosage of Botox, especially in multi‑segmental spastic patterns.
-
Bryce Charette October 11, 2025
Quick tip: When you write up a log, use consistent units – like "high/medium/low" for tone and note the activity. This makes it easier for the therapist to spot trends and adjust the program. Also, double‑check spelling of meds; a typo can cause a lot of confusion later.
-
Christina Burkhardt October 12, 2025
For anyone starting a home routine, I'd recommend setting a 5‑minute timer and focusing on one muscle group per session. Rotate daily so you cover all major joints without overwhelming the child. If you notice skin irritation from splints, pause and consult your orthotist – it's better to adjust early than to deal with breakdown later.
-
liam martin October 12, 2025
Spasticity isn’t a myth, it’s just neglected.
-
Ria Ayu October 13, 2025
When we contemplate the child's journey, we see a tapestry woven from perseverance, science, and love. Each stretch is a thread, each therapy session a color. The narrative becomes richer when families share stories, turning isolated challenges into communal wisdom. Embrace the process, for in the minutiae lies the grandeur of growth.
-
maya steele October 13, 2025
It is essential to begin with a comprehensive baseline assessment that quantifies muscle tone using the Modified Ashworth Scale, documents gait abnormalities through observational analysis, and records functional milestones such as dressing independence. From there, a multidisciplinary plan should be constructed, integrating physical therapy focused on active range of motion, strength training, and functional task practice.
Botulinum toxin injections can be strategically placed in hyperactive muscles identified via electromyography, with dosing calibrated according to body weight and muscle size to maximize efficacy while minimizing systemic exposure.
Oral antispastic agents, such as baclofen or tizanidine, may be introduced when generalized tone interferes with sleep or daily activities, but clinicians must vigilantly monitor for side effects including sedation and hypotonia.
Orthopedic interventions, including tendon lengthening or selective dorsal rhizotomy, should be reserved for cases where contractures become fixed despite conservative measures, and timing must align with skeletal maturity to prevent growth plate injury.
Home‑based regimens play a pivotal role; caregivers should be taught to perform gentle prolonged stretches, incorporate functional positioning strategies, and utilize night splints to maintain joint alignment.
Maintaining a detailed log of tone fluctuations, pain levels, and therapeutic responses enables data‑driven adjustments and empowers families to advocate effectively with insurance providers.
Interdisciplinary communication between neurologists, physiatrists, therapists, and surgeons ensures that treatment sequencing is optimized, reducing redundant interventions.
Regular re‑evaluation every six months, or sooner if clinical status changes, helps to identify emerging issues such as hip subluxation or scoliosis, which require early orthopedic referral.
Education on potential complications, including skin breakdown from orthotics and injection site bruising, prepares families to act promptly.
Finally, psychosocial support, through parent support groups and school‑based therapists, mitigates the emotional burden and fosters an inclusive environment for the child’s development.
-
Sharon Lax October 14, 2025
The guide reads like a checklist for a corporate boardroom, not a pediatric floor. Jargon overload without real‑world context makes it hard for parents to apply. A better approach would be to prioritize actionable steps and simplify the language.
-
paulette pyla October 14, 2025
Oh great, another post telling us to “just do PT” while the healthcare system decides who gets funded. Yeah, because we all have endless free time and access to elite specialists. 🙄
-
Benjamin Cook October 15, 2025
Hey folks!! Keep the momentum going!! Every tiny stretch counts!! Celebrate those micro‑wins!! You’ve got this!! 🎉
-
karthik rao October 15, 2025
While the popular narrative emphasizes “early intervention,” one must question the underlying metrics: are we truly measuring functional gain or merely compliance with institutional protocols? 🤔 A data‑driven critique reveals that many so‑called “early” programs lack longitudinal outcome studies. Hence, the blanket recommendation is, at best, an oversimplification deserving of rigorous scrutiny.
-
Breanne McNitt October 16, 2025
Let's pool our experiences: anyone who’s tried combining FES with home stretching can share what schedule works best? I’ve noticed that a 15‑minute FES session post‑PT amplifies the stretch effect.
-
Ashika Amirta varsha Balasubramanian October 16, 2025
In many South Asian cultures, caregiving is a collective duty, and families often rotate responsibilities for home exercises. Leveraging this cultural framework can improve adherence to daily stretching routines, as multiple members reinforce the habit and monitor progress.
-
Jacqueline von Zwehl October 17, 2025
For clarity, define “low,” “medium,” and “high” tone levels as follows: low – <10° resistance, medium – 10‑30°, high – >30° on the Modified Ashworth Scale. This standardization aids communication across disciplines.
-
Christopher Ellis October 17, 2025
Every limit is a horizon waiting to be redrawn.
