
DVT Risk Assessment Calculator
This tool helps you understand your personal risk of deep vein thrombosis (DVT) during long-distance travel based on factors discussed in the article. Enter your relevant medical conditions to get a personalized risk assessment and recommendations.
Traveling internationally while on blood thinners doesn’t have to be scary-but it does require smart planning. If you’re taking warfarin, rivaroxaban, apixaban, or any other anticoagulant, your biggest worry isn’t the flight itself. It’s the DVT-deep vein thrombosis-that can sneak up during long trips. The risk is real, but it’s manageable. Thousands of people fly, train, and drive long distances every year while safely on anticoagulants. The key isn’t avoiding travel. It’s knowing how to reduce your risk without overdoing it.
Why Travel Increases Your Risk of Blood Clots
Sitting still for more than four hours is the main problem. It doesn’t matter if you’re in economy, business, or first class. What matters is that your leg muscles aren’t moving. When muscles stay relaxed for too long, blood pools in your calves. That’s when clots can form. This isn’t just a myth from old airline warnings. It’s backed by data from the CDC, the American College of Chest Physicians, and the International Air Transport Association. The risk goes up with time: after 4 hours, your chance of a clot starts to rise. After 12 hours, it climbs even higher. But you’re not just at risk because you’re sitting. If you have other factors-like being over 40, having a BMI over 30, having had surgery in the last three months, or having a history of blood clots-your risk multiplies. People with active cancer, heart failure, or inherited clotting disorders like Factor V Leiden are at especially high risk. The CDC says that for travelers with two or more of these risk factors, the chance of a clot during a long trip jumps to about 1 in 1,000. That’s 5 times higher than for someone with no extra risks.What You Should NOT Do
A lot of people think they need to take extra medicine before flying. That’s a dangerous mistake. If you’re already on a therapeutic dose of an anticoagulant-meaning your doctor prescribed it to treat or prevent clots-you don’t need to take more. The American College of Chest Physicians says adding aspirin or another blood thinner won’t help. It only raises your risk of bleeding. You could end up in the ER with a stomach bleed or a brain hemorrhage because you thought you were being extra safe. Don’t skip your dose. This is one of the most common mistakes. Some people think, “I’m flying tomorrow, maybe I should skip my pill to be safer.” That’s the opposite of what you should do. Anticoagulants work by keeping your blood from clotting too easily. If you miss a dose, your blood starts to thicken again. Dr. Susan Coogan at UT Physicians says it plainly: “If you skip doses or stop taking them, your blood can actually become MORE sticky.” Don’t rely on compression socks you bought online without checking the fit. Many people buy “medical-grade” socks that say 15-20 mmHg but are actually loose or worn out. For them to work, they must fit snugly from your ankle to just below the knee. If they’re too loose, they do nothing. If they’re too tight, they can cut off circulation.What You SHOULD Do
The best defense is simple, free, and effective: move. Get up and walk every 2 to 3 hours. If you’re on a plane, walk up and down the aisle. On a bus or train, get off at stops and stretch. If you can’t get up, do seated calf exercises every 30 minutes. Tighten your calf muscles, hold for 5 seconds, then relax. Repeat 10 times. Do ankle circles. Point your toes up and down. These movements squeeze the veins in your legs and push blood back toward your heart. Wear properly fitted compression stockings. Look for below-knee graduated compression socks that provide 15-30 mmHg of pressure at the ankle. These aren’t fashion items-they’re medical devices. Ask your pharmacist or doctor to help you pick the right size. Measure your calf and ankle before buying. A bad fit is worse than no socks at all. Stay hydrated. Drink water. Not soda, not coffee, not alcohol. Alcohol and sugary drinks dehydrate you. When you’re dehydrated, your blood thickens. That’s the last thing you want. Aim for at least 8 ounces of water every hour during travel. If you’re on a 10-hour flight, that’s 80 ounces. Bring an empty bottle through security and fill it up.
Managing Your Medication While Traveling
If you’re on warfarin, you need to plan ahead. Warfarin’s effect is measured by your INR-a number that tells how long your blood takes to clot. Your doctor should check your INR 1 to 2 weeks before you leave. The target range depends on why you’re on it: 2.0-3.0 for atrial fibrillation, 2.5-3.5 for mechanical heart valves. If your INR is too low, you’re at risk for clots. Too high, and you risk bleeding. If you’re traveling for more than two weeks and your INR has been unstable, consider a portable INR monitor. The Roche CoaguChek® Mobile costs around $299, and each test strip is about $7.50. It’s worth it if you’ve had trouble keeping your INR steady. You can test yourself in your hotel room and call your doctor if it’s out of range. Time zones matter. If you’re taking warfarin once a day, take it at the same clock time, not the same circadian time. If you normally take it at 7 p.m. in New York and fly to London (5 hours ahead), take it at 7 p.m. London time. Don’t shift to 2 a.m. your old time. That throws off your schedule and increases the chance of a missed dose. If you’re on a DOAC-like rivaroxaban, apixaban, or dabigatran-you’re luckier. No blood tests. No food restrictions. Just take it at the same time every day. Rivaroxaban is taken with food, so plan meals around it. If you forget a dose, take it as soon as you remember, unless it’s almost time for the next one. Never double up.What to Pack
Don’t just throw your pills in your suitcase. Bring your medication in its original bottle with the pharmacy label. Carry a copy of your prescription and a letter from your doctor listing your medications, dosages, and diagnosis. This helps if you’re stopped at customs or need emergency care abroad. Check if your medication is available where you’re going. Apixaban and rivaroxaban aren’t sold in 32% of low-income countries, according to the WHO. If you’re going somewhere remote, bring extra-enough for your whole trip plus a few extra days. Store DOACs at room temperature. LMWH (like dalteparin) needs refrigeration. If you’re flying with injections, bring a cooler with ice packs and a doctor’s note explaining why you need them. Pack a small emergency kit: a list of symptoms to watch for, contact info for your doctor back home, and the nearest hospital or clinic at your destination. Know the signs of a clot: swelling in one leg, redness, warmth, or pain. Know the signs of a pulmonary embolism: sudden shortness of breath, sharp chest pain when you breathe, rapid heartbeat.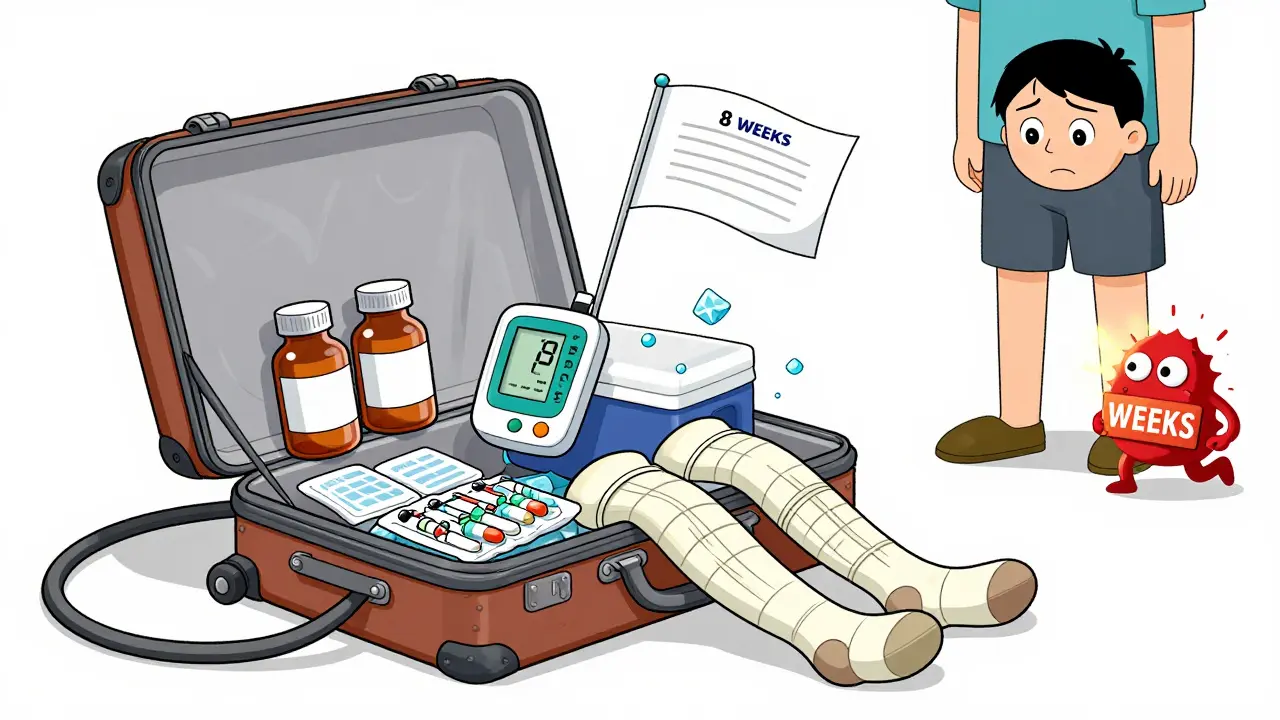
When to Avoid Travel
The IATA Medical Manual says you can fly if you’ve had a DVT and are now asymptomatic and stable on anticoagulants. That’s good news. But some hospitals, like Cambridge University Hospitals, advise against long trips within four weeks of a clot. There’s no universal rule. If you’ve had a recent clot, talk to your doctor. Don’t rely on airline policies. Your doctor knows your history. If you’ve had major surgery in the last month-especially under general anesthesia-or if you have active cancer, your risk is high. Even with anticoagulants, your body is still healing. Your doctor might suggest delaying travel. If you must go, they may recommend a single dose of LMWH before departure. Rivaroxaban 10 mg taken one to two hours before travel is another option, but only if your doctor approves it.What to Do If You Think You Have a Clot
Don’t wait. If you notice swelling in one leg, especially if it’s painful, warm, or red, get medical help immediately. DVT can turn into a pulmonary embolism-a clot that travels to your lungs. That’s life-threatening. If you have sudden shortness of breath, chest pain that gets worse when you breathe, or cough up blood, call emergency services. Don’t try to drive yourself. Remember: clots can develop up to eight weeks after travel. That’s not a typo. You’re not safe just because you’re home. Keep watching for symptoms for at least two months after your trip.Bottom Line: You Can Travel Safely
About 4 million Americans are on long-term anticoagulants. Around 65% of them travel each year. Most do it without a problem. The secret isn’t avoiding flights or skipping meds. It’s knowing the risks and taking simple, proven steps: move often, wear the right socks, stay hydrated, take your pills on time, and pack smart. You don’t need to be afraid. You just need to be prepared.Can I fly after having a deep vein thrombosis (DVT)?
Yes, you can fly after a DVT if you’re asymptomatic and stable on anticoagulant therapy. The International Air Transport Association (IATA) allows air travel once the patient is no longer in pain, has no swelling, and is on a consistent anticoagulant regimen. However, some hospitals recommend waiting at least four weeks after diagnosis to reduce the risk of recurrence. Always consult your doctor before flying, especially if your DVT was recent or unprovoked.
Should I take aspirin before a long flight while on blood thinners?
No. Taking aspirin while already on a therapeutic anticoagulant like warfarin, rivaroxaban, or apixaban increases your risk of bleeding without reducing your risk of clots. The American College of Chest Physicians specifically advises against adding aspirin or other extra anticoagulants for travel. The only proven non-drug prevention methods are movement, compression stockings, and hydration.
Do I need to get my INR checked before traveling if I’m on warfarin?
Yes. If you’re on warfarin, get your INR tested 1 to 2 weeks before departure. Your target range depends on your condition-usually 2.0-3.0 for atrial fibrillation or 2.5-3.5 for mechanical heart valves. If your INR is too low, you’re at risk for clots. Too high, and you risk bleeding. If your INR is unstable or you’re traveling for more than two weeks, consider bringing a portable INR monitor like the Roche CoaguChek® Mobile.
Are compression socks necessary for everyone on anticoagulants?
Not for everyone, but recommended for high-risk travelers. If you have one or more risk factors-like age over 40, obesity, recent surgery, cancer, or a history of clots-wearing properly fitted 15-30 mmHg graduated compression stockings is advised by the CDC and ACCP. For low-risk travelers, movement and hydration are enough. Make sure the socks fit snugly; loose socks don’t help and can even be harmful.
Can I bring my blood thinner on an international flight?
Yes. Keep all medications in their original containers with pharmacy labels. Carry a copy of your prescription and a doctor’s note listing your medications and diagnosis. For injectables like LMWH, bring a cooler with ice packs and a letter explaining medical necessity. DOACs like rivaroxaban can be packed in carry-on luggage at room temperature. Check if your medication is available at your destination-some DOACs aren’t sold in low-income countries.
How long after travel should I watch for signs of a clot?
Up to eight weeks. Blood clots can develop long after you’ve returned home. Watch for swelling, pain, or redness in one leg. Also watch for sudden shortness of breath, chest pain, or coughing up blood. These could mean a clot has traveled to your lungs. Don’t ignore symptoms just because you’re home. Seek medical help immediately if you notice any warning signs.
Comments (14)
-
Jasmine Yule December 30, 2025
This post is a lifesaver. I’ve been on apixaban for AFib and was terrified to fly to Bali last year. I did the calf exercises every 30 minutes, wore my compression socks (got them fitted at CVS, not Amazon), and drank a water bottle every hour. No clot, no drama. Just a very sore calf and a whole lot of gratitude.
Also, don’t buy those ‘medical grade’ socks on Etsy. They’re not. I learned the hard way. Measure your ankle and calf. Seriously.
And yes - NO ASPIRIN. I had a cousin who did that and ended up in the ER with a GI bleed. Don’t be that person.
-
Manan Pandya December 30, 2025
Excellent breakdown. The distinction between DOACs and warfarin regarding time zone management is particularly well-articulated. Many patients assume circadian rhythm dictates dosing, but pharmacokinetics demand chronometric consistency. A 7 p.m. dose in New York must remain a 7 p.m. dose in London - not 2 a.m. local time. This oversight is a leading cause of INR fluctuations in international travelers.
-
Aliza Efraimov December 31, 2025
OMG I CRIED READING THIS. I had a PE after a 14-hour flight two years ago. I thought I was fine because I was on warfarin. I skipped my dose because I was ‘too busy.’ Turns out, skipping = sticky blood. I spent three days in ICU. My mom flew over and found me sobbing because I couldn’t breathe.
Don’t skip. Don’t wing it. Don’t be like me. Move. Hydrate. Wear the damn socks. I now carry a little note in my wallet that says ‘I’m on blood thinners - if I collapse, call 911 and tell them I’m on apixaban.’
Thank you for writing this. I wish I’d had it before my flight.
-
Nisha Marwaha January 2, 2026
From a hematology standpoint, the risk stratification presented here aligns with the 2021 ACCP guidelines on venous thromboembolism prophylaxis in travelers. The 1-in-1,000 risk threshold for multivariate risk factors (age, BMI, recent surgery, prior VTE) is empirically validated. However, the recommendation for portable INR monitoring is underemphasized. For patients with unstable INR trajectories, self-monitoring with CoaguChek® reduces hospitalizations by 42% per the PROTEUS trial. Also, note that LMWH requires cold chain maintenance - refrigeration at 2–8°C is non-negotiable for stability. Room temperature exposure >24h may degrade bioavailability.
-
Paige Shipe January 3, 2026
So let me get this straight. You’re telling me I can’t drink wine on my trip to Italy? And I have to walk around the plane like a zombie? And wear socks that look like they’re meant for a diabetic grandma? And I can’t skip my pill because I’m ‘feeling fine’?
What’s the point of traveling if I can’t even enjoy myself? I’m on blood thinners, not in prison. I’ll take my chances. At least I’ll die with a glass of Chianti in my hand.
-
Tamar Dunlop January 4, 2026
Thank you for this meticulously composed and profoundly considerate guide. As a Canadian physician who has treated numerous international travelers on anticoagulants, I can attest to the precision of your recommendations. The emphasis on hydration over alcohol consumption, the critical importance of properly fitted graduated compression stockings, and the nuanced guidance regarding DOAC dosing across time zones are not merely prudent - they are life-preserving. I shall be distributing this to all my patients embarking on long-haul journeys. A truly exemplary piece of patient education.
-
David Chase January 6, 2026
WHY IS EVERYONE SO SCARED OF A LITTLE BLOOD CLOT?!?!!??!??
Look - I’ve flown 47 times in the last year. I’m 32, fit, and on rivaroxaban. I drink beer on the plane. I don’t move. I don’t wear socks. I skip my pill once a week because I forget. I’m fine. Everyone else is just weak. You think you’re special? You’re not. You’re just scared of flying because you’ve been told to be. The real danger? Being so paranoid you never leave your house.
PS: I just bought 10 pairs of ‘compression socks’ off Amazon. They’re cute. I wear them with my sneakers. I’m a legend.
💯🔥 #TravelHard #BloodThinnerBoss
-
Emma Duquemin January 8, 2026
I did a 16-hour flight from LA to Sydney on apixaban and lived to tell the tale - and I did it with style. I walked the aisle every hour like I was on a runway show. I did ankle circles like I was auditioning for Swan Lake. I drank water like it was my job. I even packed a little playlist called ‘Calf Pump Hits’ - think ‘Eye of the Tiger’ mixed with yoga beats.
And guess what? My leg didn’t turn into a sausage. My feet didn’t explode. I didn’t need a miracle. I just followed the damn plan.
To anyone reading this and thinking, ‘I’m too cool for socks’ - you’re not cool. You’re a walking blood clot waiting for a TSA agent to ask you if you’re okay.
Be smart. Be bold. Be alive. Move. Hydrate. Live.
-
Kevin Lopez January 10, 2026
DOACs don’t need INR. Warfarin does. Compression socks: 15-30 mmHg. No aspirin. Hydrate. Move. That’s it. Everything else is noise. You’re overcomplicating it. Do the basics. Don’t be a statistic.
-
Duncan Careless January 11, 2026
Good advice overall, though I’d suggest adding a note about airport security. I’ve had my LMWH syringes flagged twice because the label was faded. Always carry the doctor’s letter in a plastic sleeve - and maybe a printed copy of the WHO guidelines on medication transport. It helps. Also, don’t forget to check if your destination has a pharmacy that stocks your DOAC. I once had to fly to Bali with only 3 days’ supply because the local chemist didn’t carry rivaroxaban. Panicked for a week.
-
Samar Khan January 12, 2026
LMAO you people are so dramatic. I had a DVT and flew to India anyway. I didn’t even drink water. I took my pill when I remembered. And guess what? I’m still here. You’re all just scared of your own shadows. Also, compression socks? I wear my yoga pants. Same thing. 😘
-
Russell Thomas January 13, 2026
Wow. So let me get this straight - you want me to walk around like a robot, drink water like it’s my job, and wear socks that make me look like I’m in a 1980s hospital drama… all because some doctor told you to?
What if I just… don’t care?
What if I’d rather die on a beach in Thailand than live my life in fear of a clot?
Oh wait - you’re one of those people who thinks you’re ‘safe’ because you followed a blog post.
Pathetic.
-
Joe Kwon January 14, 2026
This is such a well-researched, balanced piece. I’ve been on warfarin for 8 years and fly internationally twice a year. The portable INR monitor was a game-changer - I tested in my hotel in Tokyo and adjusted my dose before flying home. Saved me a hospital trip.
Also, the time zone advice? Spot on. I used to take my pill at 7 p.m. New York time, even when I was in Bangkok. My INR went haywire. Now I use my phone’s clock. Simple. Life-changing.
And yes - no aspirin. I learned that the hard way after a nosebleed that lasted 45 minutes. Never again.
-
Nicole K. January 15, 2026
You’re telling people to drink water and move? That’s it? No pills? No magic? You’re just telling people to be healthy? How lazy. I’ve been on blood thinners for 15 years and I take 12 supplements a day. You’re just encouraging laziness.
