Transplant Medication: What You Need to Know
When working with transplant medication, drugs prescribed to stop the immune system from attacking a newly‑placed organ. Also known as anti‑rejection therapy, it plays a critical role in keeping transplants alive and patients healthy.
One of the core immunosuppressant, a class of medicines that calm the body’s defense mechanisms is Tacrolimus, a calcineurin inhibitor widely used after kidney, liver and heart transplants. Another staple is Mycophenolate Mofetil, an antiproliferative agent that blocks immune cell growth. Together these agents form a layered approach: they reduce rejection risk, allow lower doses of each drug, and minimize side‑effects when balanced correctly.
Why does this matter? Transplant medication isn’t a one‑size‑fits‑all product; each organ, patient age and health status shapes the drug mix. For example, liver recipients often start with higher Tacrolimus levels because the liver clears the drug faster, while heart patients may rely more on Cyclosporine for its proven cardiac outcomes. Understanding these nuances helps you ask the right questions at follow‑up appointments.
Key Factors That Influence the Choice of Anti‑Rejection Drugs
The first factor is organ type. Kidneys, livers, hearts and lungs each have distinct immune triggers, so the drug cocktail varies. Second, genetic background matters—a patient’s CYP3A5 genotype can make Tacrolimus clear faster or slower, which directly impacts dosing.
Third, side‑effect profile. Immunosuppressants can raise blood pressure, cause kidney toxicity, or increase infection risk. Monitoring labs like serum creatinine, liver enzymes and blood sugar helps catch problems early. Fourth, drug interactions. Many antibiotics, antifungals and even over‑the‑counter supplements can push drug levels too high, risking toxicity.
All these pieces form a semantic chain: organ type influences drug selection, genetics affect dosing, and lab monitoring guides adjustments. This chain is the backbone of personalized transplant care.
Practical tip: keep a medication journal. Write down each dose, the time taken, and any new symptoms. Bring this record to every clinic visit. Clinicians can spot trends—like a sudden rise in blood pressure after adding a new antibiotic—and tweak the regimen before serious issues develop.
Another crucial element is adherence. Missing doses can spike rejection rates dramatically. Studies show that patients who skip just one dose per week have a two‑fold higher chance of acute rejection. Setting phone alarms, using pill boxes, or syncing with a health app can keep you on track.
When you first start on transplant medication, expect a period of frequent blood tests. Initial weeks may involve weekly draws to fine‑tune Tacrolimus trough levels (usually 5‑15 ng/mL depending on the organ). After stabilization, testing often shifts to monthly or quarterly, but any infection, new medication, or illness can trigger a re‑check.
Let’s not forget the long‑term picture. Over years, the immune system can become less reactive, allowing doctors to safely lower doses. Conversely, chronic kidney disease can develop from prolonged calcineurin inhibitor use, prompting a switch to newer agents like Belatacept. Staying informed about emerging therapies lets you discuss options with your transplant team.
Beyond the drugs themselves, lifestyle plays a supportive role. A balanced diet low in sodium helps control blood pressure, while regular moderate exercise improves overall health and reduces infection risk. Avoiding smoking and limiting alcohol also protect the transplanted organ.
If you experience side effects—tremors, gum overgrowth, or unusual bruising—don’t wait. Contact your transplant coordinator promptly. Often a simple dose adjustment or adding a protective medication (e.g., antihypertensives or antifungals) can resolve the issue without compromising rejection protection.
Finally, mental health matters. The stress of managing a complex medication schedule can feel overwhelming. Many transplant centers offer counseling or support groups where you can share experiences, learn coping strategies, and stay motivated to stick with the regimen.
In the collection below you’ll find deep‑dive articles on specific drugs, practical guides for dosing, side‑effect management, and the latest research on emerging anti‑rejection therapies. Whether you’re a new transplant recipient or a caregiver looking for clear answers, these resources are organized to help you navigate the world of transplant medication with confidence.
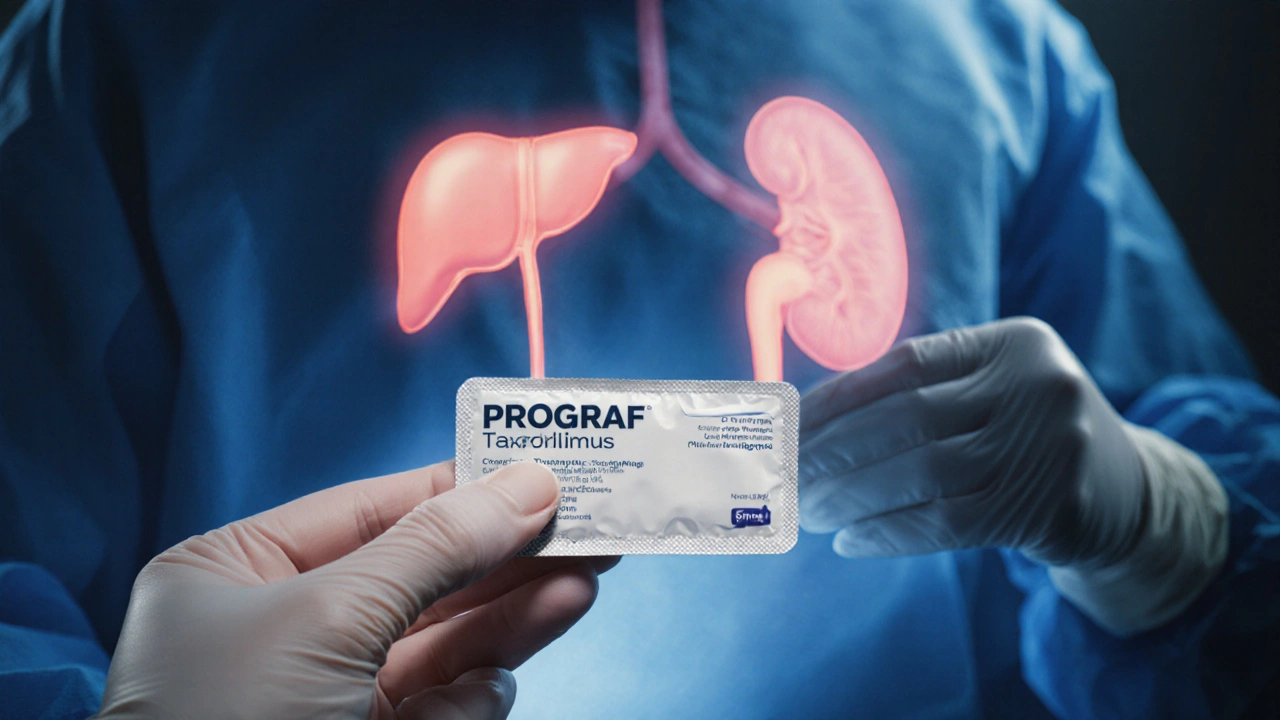
Prograf (Tacrolimus) vs. Alternatives: A Practical Comparison Guide
Haig Sandavol Oct 5 19A clear, side‑by‑side comparison of Prograf (Tacrolimus) with top alternatives, covering how they work, side effects, costs, and how to choose the right option.
More Detail