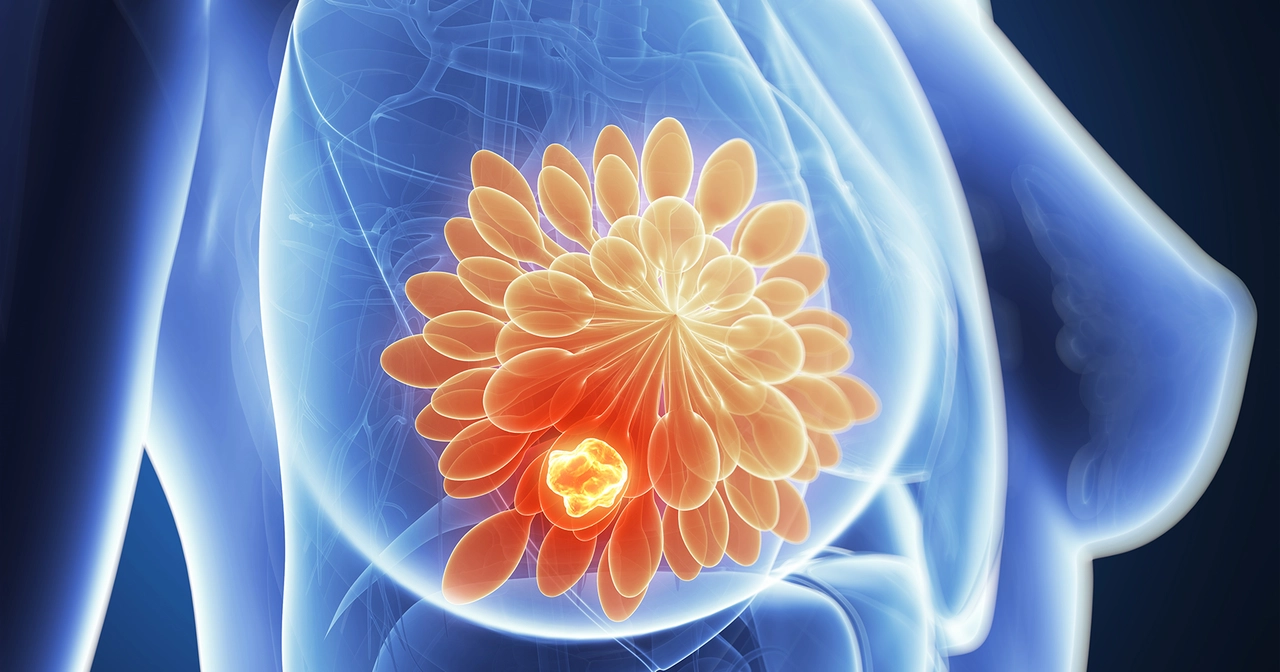
Breast cancer: what to watch for and what to do next
Worried about breast cancer? You're not alone. Knowing the common signs, when to get checked, and what treatment choices look like can make a big difference. This page gives clear, practical steps you can use right now — whether you're checking yourself or helping someone you care about.
Signs and early red flags
Not every lump is cancer, but any new breast change should be checked. Look for a hard lump, thickening under the skin, one breast looking different from the other, dimpling, nipple discharge (not milk), or a new sore that doesn’t heal. Also pay attention to persistent pain in one area — pain alone is less common as a first sign, but it still matters.
If you notice any of these, schedule an appointment with your primary care doctor or a breast specialist. Early checks mean more options and usually better outcomes.
Screening and diagnosis
Screening catches cancer before symptoms appear. Mammograms are the main tool: they’re quick and recommended at regular intervals based on age and risk. If you have a strong family history or known gene changes (like BRCA), your doctor may suggest earlier or additional screening such as MRI or ultrasound.
If screening or an exam finds something suspicious, the next steps often include diagnostic imaging and a biopsy. A biopsy is the only way to confirm cancer. Pathology results tell doctors the type of tumor and whether hormone receptors or other markers are present — that info guides treatment.
Treatment options and support
Treatment depends on the cancer type, size, and whether it spread. Common approaches are surgery (lumpectomy or mastectomy), radiation, chemotherapy, hormone therapy for estrogen/progesterone-positive cancers, and targeted therapies for specific markers. Many people get a combination of these treatments. Your team will explain the goals, side effects, and timeline so you can make informed choices.
Side effects and recovery vary. Ask about fertility preservation if you’re of childbearing age, and get a clear plan for managing nausea, fatigue, and other symptoms. Rehab, lymphedema prevention, and side-effect clinics can help during and after treatment.
Facing breast cancer can feel overwhelming. Reach out to support groups, a counselor, or a patient navigator — they help with appointments, insurance questions, and emotional support. Practical help like meal delivery, transport to treatments, and childcare can reduce stress and let you focus on care.
Action steps: do a monthly self-check, follow screening advice for your age and risk, and see your doctor for any new breast changes. Keep questions ready for visits: ask about type, stage, treatment options, likely side effects, and next steps. Small actions now can change the path later.
If you want links to reliable resources, screening guidelines, or a short checklist to take to your doctor, we can put those together for you. Just ask and we’ll help you find practical next steps.
Anastrozole and Quality of Life: What You Need to Know
Haig Sandavol Apr 27 18Anastrozole is a medication I came across recently that is often prescribed to postmenopausal women with hormone receptor-positive breast cancer. It works by reducing the production of estrogen, a hormone that can stimulate the growth of certain breast cancer cells. I've learned that this drug has a significant impact on the quality of life for many patients, as it can cause side effects like hot flashes, joint pain, and mood changes. It's important to talk to your doctor about any concerns you may have, as there are strategies and resources available to help manage these side effects. In the end, the benefits of Anastrozole in treating breast cancer often outweigh the challenges, but being informed and knowing what to expect can make all the difference in your journey.
More Detail