
Osteodystrophy Prevention Calculator
Calculate your daily vitamin D and calcium needs based on your age, vitamin D levels, and health conditions.
When you hear the wordosteodystrophy, you might think of a rare bone disorder that only doctors talk about. In reality, it’s becoming a common problem for millions of seniors, and it’s tied directly to the way our bodies change as we age. This article breaks down what osteodystrophy is, why older adults are especially vulnerable, how you can spot it early, and what steps can keep bones strong well into later years.
Key Takeaways
- Osteodystrophy describes abnormal bone mineralization caused by metabolic imbalances, often linked to aging.
- Reduced calcium absorption, vitamin D deficiency, and chronic kidney disease are the top drivers in seniors.
- Early detection with a bone density test (DEXA) can prevent fractures and preserve independence.
- Nutrition, weight‑bearing exercise, and careful medication management are the cornerstones of treatment.
- Public‑health policies that target bone health can curb the growing economic burden of falls and fractures.
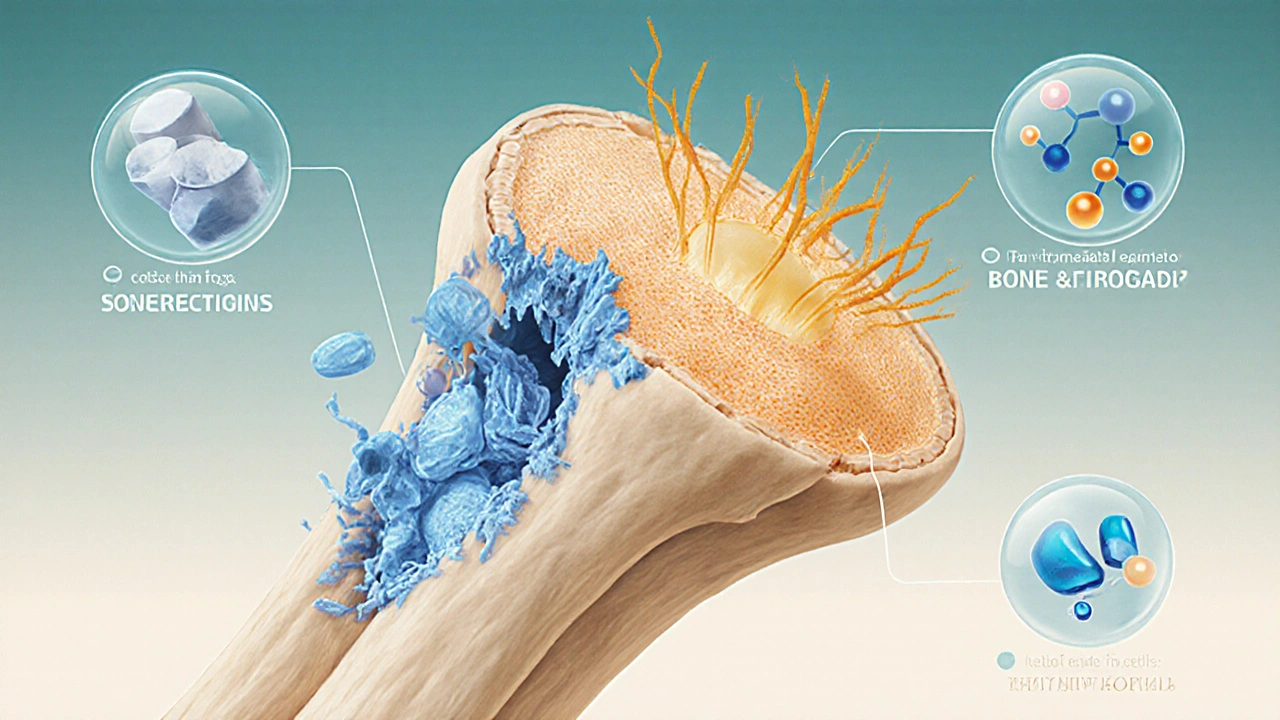
Osteodystrophy is a disorder of bone development and remodeling that results in weakened, poorly mineralized bone tissue. It can arise from a range of metabolic disturbances, including hormone imbalances, chronic kidney disease, and nutritional deficiencies. While the term covers several specific conditions-such as renal osteodystrophy and osteomalacia-its common thread is disrupted bone health.
Aging Population refers to the growing share of people aged 65 and older worldwide. In the United States, seniors now make up about 17% of the total population, and that proportion is expected to exceed 22% by 2035. As the demographic shifts, age‑related bone disorders become a public‑health priority.
Why Bones Get Weaker With Age
Bone is a living tissue that constantly remodels itself through a balance of resorption (breakdown) and formation. This process, called Bone Remodeling a cycle where osteoclasts remove old bone and osteoblasts lay down new matrix, is tightly regulated by minerals, hormones, and mechanical loading.
With advancing age, several key elements of this system start to falter:
- Calcium Metabolism becomes less efficient. The gut absorbs less calcium, and the kidneys excrete more, leading to a net deficit.
- Vitamin D Deficiency skyrockets because skin synthesis declines and older adults often spend less time outdoors.
- Levels of Parathyroid Hormone a hormone that raises blood calcium by stimulating bone resorption rise in response to low calcium, accelerating bone loss.
- Many seniors develop Chronic Kidney Disease a condition that reduces the kidneys' ability to activate vitamin D and excrete phosphate, further disrupting mineral balance.
These shifts tip the remodeling balance toward resorption, creating the perfect storm for osteodystrophy.
Major Causes of Osteodystrophy in Older Adults
Reduced Calcium Absorption: After age 50, intestinal calcium absorption can drop by up to 30%. Even with adequate dietary intake, the net calcium available for bone formation shrinks.
Vitamin D Deficiency: Serum 25‑hydroxy‑vitamin D levels below 20ng/mL are common in seniors. This deficiency impairs calcium absorption and suppresses the production of active vitamin D (calcitriol) by the kidneys.
Renal Osteodystrophy: In patients with Chronic Kidney Disease, phosphate retention and reduced calcitriol trigger secondary hyperparathyroidism, which leads to high‑turnover bone disease.
Hormonal Changes: Post‑menopausal women experience a sharp decline in estrogen, a hormone that protects bone. Men also see a gradual drop in testosterone, contributing to bone loss.
Lifestyle Factors: Sedentary behavior, smoking, and excessive alcohol intake all impair bone formation. Conversely, weight‑bearing activities stimulate osteoblast activity.
Recognizing Symptoms & Getting a Diagnosis
The early stages of osteodystrophy are often silent. The first clue may be a low‑impact fracture-a wrist, hip, or vertebral break after a minor stumble. Persistent bone pain, especially in the ribs, pelvis, or long bones, can also signal the problem.
Clinicians rely on a combination of lab tests and imaging:
- Serum calcium, phosphate, and alkaline phosphatase levels to gauge bone turnover.
- 25‑hydroxy‑vitamin D concentration for deficiency assessment.
- Intact Parathyroid Hormone measurement to detect secondary hyperparathyroidism.
The definitive imaging tool is the Bone Density Test (DEXA) dual‑energy X‑ray absorptiometry that measures bone mineral density at the hip and spine. A T‑score of -2.5 or lower confirms osteoporosis, a common endpoint of untreated osteodystrophy.
Management Strategies That Work
Effective care blends medical treatment, nutrition, and physical activity. Here’s a practical roadmap:
- Optimize Calcium Intake: Aim for 1,200mg per day from dairy, leafy greens, fortified foods, or supplements. Split the dose to improve absorption.
- Correct Vitamin D Levels: Most seniors need 800-1,000IU of vitaminD3 daily, with higher doses (2,000-4,000IU) if serum 25‑OH‑D is severely low.
- Address Underlying Conditions: Manage chronic kidney disease, adjust medications that affect bone (e.g., glucocorticoids), and treat secondary hyperparathyroidism with phosphate binders or calcimimetics.
- Pharmacologic Options: Bisphosphonates (alendronate, risedronate) inhibit bone resorption; denosumab offers a 6‑month injectable alternative; anabolic agents like teriparatide can rebuild bone in high‑risk patients.
- Weight‑Bearing Exercise: Activities such as brisk walking, stair climbing, resistance training, and tai chi improve bone density and balance, reducing fall risk.
- Fall‑Prevention Measures: Home safety audits (grab bars, non‑slip mats), vision checks, and balance‑training programs can cut fracture rates dramatically.
Regular follow‑up with a healthcare provider ensures that bone density is monitored and treatment adjusted as needed.

Public‑Health Implications and Future Outlook
By 2030, the United States is projected to spend $60billion annually on fracture‑related care, most of which stems from osteodystrophy and osteoporosis in older adults. Investing in early detection and preventive programs could save billions and preserve quality of life.
Emerging research points to novel biomarkers-such as sclerostin and fibroblast growth factor‑23-that may predict bone loss before a fracture occurs. Telehealth platforms are also expanding access to bone‑health education, especially in rural areas.
Community‑level actions, like vaccination against influenza (which reduces inflammatory bone loss) and nutrition assistance programs that provide calcium‑rich foods, are low‑cost ways to support skeletal health across the aging population.
Quick Checklist for Seniors and Caregivers
- Get a DEXA scan if you’re 65+ or 50+ with risk factors.
- Check serum vitaminD every 2years; supplement as needed.
- Consume at least 1,200mg of calcium daily.
- Incorporate weight‑bearing exercise 3 times a week.
- Review medications with a pharmacist to spot bone‑weakening drugs.
- Make home safety modifications to prevent falls.
Understanding and acting on these steps can keep osteodystrophy from turning into a disabling condition. The good news? Bones respond to change at any age, and even modest lifestyle tweaks can make a huge difference.
Frequently Asked Questions
How is osteodystrophy different from osteoporosis?
Osteodystrophy is a broader term that covers any bone disorder caused by metabolic problems, such as vitaminD deficiency or kidney disease. Osteoporosis specifically describes low bone mass and structural deterioration, usually due to age‑related hormonal changes. All osteoporosis is a form of osteodystrophy, but not all osteodystrophy is osteoporosis.
Can a DEXA scan detect osteodystrophy early?
DXA measures bone mineral density, which drops before fractures occur. While it doesn’t pinpoint the underlying metabolic cause, a low T‑score flags the need for further labs (calcium, vitaminD, PTH) to diagnose osteodystrophy.
Is calcium supplementation enough to prevent bone loss?
Calcium is essential, but without adequate vitaminD, the body can’t absorb it efficiently. A combined approach-diet, vitaminD, and regular exercise-offers the best protection.
What role does chronic kidney disease play?
CKD reduces the kidneys’ ability to convert vitaminD to its active form and leads to phosphate buildup. Both changes drive secondary hyperparathyroidism, accelerating bone turnover and causing renal osteodystrophy.
Are there new treatments on the horizon?
Researchers are testing sclerostin‑inhibiting antibodies that boost bone formation, and gene‑therapy approaches that may correct metabolic defects at their source. While still experimental, these could change management in the next decade.
Comments (11)
-
Ben Poulson October 13, 2025
Thank you for the comprehensive overview; the connection between reduced calcium absorption and the increased prevalence of osteodystrophy in seniors is particularly noteworthy. It is essential that clinicians monitor serum calcium and vitamin D levels routinely, especially in patients over the age of sixty‑five. Moreover, incorporating bone‑density testing into standard geriatric assessments can facilitate early intervention. Your emphasis on weight‑bearing exercise and fall‑prevention strategies aligns well with current best‑practice guidelines. Overall, the article provides a solid framework for both clinicians and caregivers.
-
Raghav Narayan October 18, 2025
First and foremost, it is imperative to recognize that osteodystrophy is not merely a singular disease entity but rather a spectrum of metabolic bone disorders that share common pathophysiological mechanisms. The gradual decline in intestinal calcium absorption after the fifth decade, coupled with the age‑related reduction in cutaneous synthesis of vitamin D, creates a perfect milieu for mineral imbalances. In addition to these physiological changes, many older adults develop chronic kidney disease, which further impairs the activation of 25‑hydroxy‑vitamin D to its biologically active form, calcitriol. This cascade results in secondary hyperparathyroidism, a condition wherein elevated parathyroid hormone accelerates bone resorption to maintain serum calcium levels. Consequently, the net effect is a shift toward bone loss that predisposes individuals to fractures even after low‑impact falls. To mitigate these risks, a multifaceted approach is required, beginning with a thorough dietary assessment to ensure a daily calcium intake of approximately 1,200 mg, preferably obtained from a combination of dairy products, leafy greens, and fortified foods. Simultaneously, serum 25‑hydroxy‑vitamin D should be measured at least biennially, with supplementation ranging from 800 to 2,000 IU of vitamin D₃ daily, adjusted according to baseline levels. For patients with proven deficiency, higher loading doses-such as 50,000 IU weekly for eight weeks-may be warranted, followed by maintenance therapy. Pharmacologic intervention should be considered when lifestyle measures alone prove insufficient; bisphosphonates remain the first‑line agents for reducing osteoclastic activity, yet clinicians must be vigilant for potential adverse effects, including esophageal irritation and atypical femoral fractures. In cases where bisphosphonate therapy is contraindicated or ineffective, denosumab offers a subcutaneous alternative with a biannual dosing schedule, while teriparatide may be employed for anabolic stimulation of bone formation in high‑risk patients. Regular follow‑up, ideally every twelve months, should include repeat DEXA scanning to assess changes in bone mineral density, as well as periodic laboratory monitoring of calcium, phosphate, PTH, and vitamin D metabolites. Finally, patient education is a cornerstone of successful management; individuals must understand the importance of adherence to supplementation, the role of resistance training and walking in stimulating osteoblasts, and the necessity of home‑environment modifications to reduce fall hazards. By integrating these evidence‑based strategies, healthcare providers can substantially diminish the burden of osteodystrophy within the aging population.
-
Tara Phillips October 24, 2025
Your enthusiasm for proactive bone health is admirable; emphasizing early screening and consistent supplementation can indeed transform outcomes for many seniors. The recommendation to aim for at least 1,200 mg of calcium daily, paired with 800–1,000 IU of vitamin D, provides a clear, actionable target. Moreover, encouraging regular weight‑bearing activities such as brisk walking or light resistance training aligns perfectly with the physiological need to stimulate osteoblastic activity. Lastly, the reminder to review medication regimens for potential bone‑depleting agents underscores the comprehensive nature of optimal care.
-
Derrick Blount October 29, 2025
While the article certainly elucidates the relationship between calcium deficiency and osteodystrophy, one must also consider the concomitant impact of sedentary lifestyles, dietary inadequacies, and, importantly, the pharmacological agents-such as glucocorticoids-that exacerbate bone resorption; additionally, the role of chronic inflammation, often overlooked, warrants further discussion, as it contributes to osteoclast activation, thereby accelerating skeletal deterioration.
-
Anna Graf November 4, 2025
Bones are like the foundations of a house; if the ground shifts, the whole structure feels it. So caring for them early keeps the whole life sturdy.
-
Jarrod Benson November 9, 2025
Wow, this piece really hits the nail on the head-bone health isn’t something you can just forget about once you hit retirement, you gotta stay on top of it! I’ve been hitting the local community center three times a week, doing a mix of resistance bands, squats, and even a bit of dancing, and I swear I feel stronger already. Adding in a solid calcium‑rich breakfast-think oatmeal with almond milk and a splash of orange juice-keeps my morning smooth, and I never skip my vitamin D supplement because I know the sunshine isn’t always reliable. The article’s reminder to check those labs every couple of years is spot‑on; my doc caught my low vitamin D last winter and we bumped up the dose, which made a huge difference in my energy levels. Plus, the fall‑prevention tips are gold-simple stuff like sturdy night‑lights and non‑slip mats can save you a broken hip later. All in all, staying active, eating right, and keeping those check‑ups regular is the winning combo for keeping our skeletons in good shape as we age.
-
Liz . November 14, 2025
Totally agree with you the community center workouts are a game changer and those night lights really help avoid those scary slips
-
tom tatomi November 20, 2025
Monitoring vitamin D levels remains essential.
-
Tom Haymes November 25, 2025
Indeed, regular assessment of serum 25‑hydroxy‑vitamin D provides a reliable baseline from which clinicians can tailor supplementation, thereby optimizing calcium absorption and minimizing the risk of secondary hyperparathyroidism.
-
Scott Kohler December 1, 2025
One might wonder why the “official” guidelines emphasize calcium and vitamin D without mentioning the hidden agenda of the supplement industry, whose profit motives could well be steering public health recommendations toward perpetual consumer dependence.
-
Brittany McGuigan December 6, 2025
The articel clearly demonstrates the need for early detection, yet many healthcare system still lag behind in implementing widespread DEXA screening programs, which is a real failur for patient outcomes.
