
Diuretic Selection Tool
Select your clinical scenario to find the most appropriate diuretic. Based on the article content, this tool helps you choose between Furosemide and its alternatives considering key factors like kidney function, indication, and patient-specific needs.
Patient Scenario
Patient Factors
Dealing with fluid buildup can feel like trying to empty a bathtub with a leaky plug. That's where diuretics step in, helping the body flush excess water and salts. If you’ve been prescribed a water‑pushing medication, you’ve probably heard the name Furosemide. But is it always the right choice? Let’s compare it with the most common alternatives so you can understand when each one shines and when it falls short.
What is Furosemide?
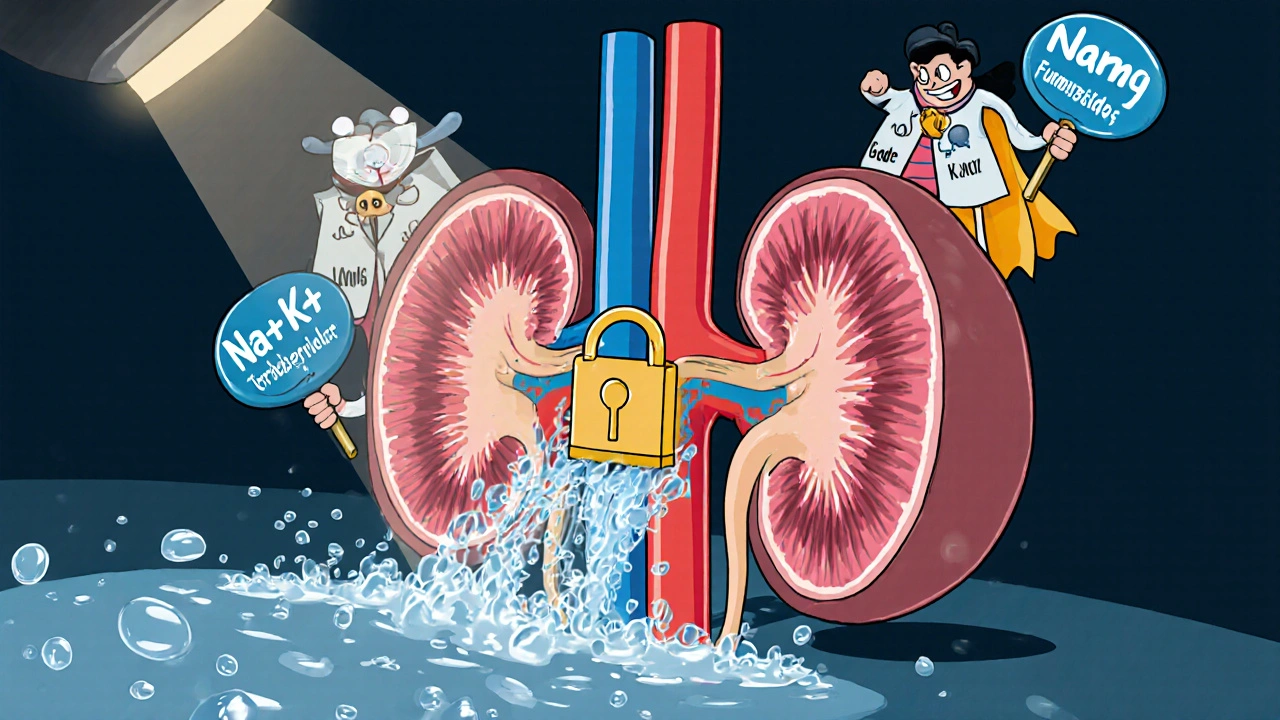
Furosemide belongs to the loop diuretic class, named after the part of the kidney loop of Henle where it acts. It blocks the Na⁺‑K⁺‑2Cl⁻ cotransporter, preventing sodium, chloride, and water from being reabsorbed. The result: a rapid, high‑volume urine output. Doctors often turn to it for heart failure, pulmonary edema, or severe hypertension when a quick fluid reduction is needed.
How Loop Diuretics Work (and Why They’re Powerful)
Loop diuretics-including Furosemide, Bumetanide, Torsemide, and Ethacrynic acid-target the thick ascending limb of the loop of Henle. By shutting down that cotransporter, they cause a loss of about 15‑20 % of the filtered sodium load, far more than thiazide diuretics, which affect only 5‑10 % in the distal tubule. This makes loops the most potent diuretics available, but the potency also brings a higher risk of electrolyte shifts.
Major Alternatives to Furosemide
While Furosemide is the go‑to, clinicians sometimes reach for other agents based on patient tolerance, cost, or specific clinical scenarios.
Hydrochlorothiazide (Thiazide Diuretic)
Hydrochlorothiazide (HCTZ) works farther down the nephron, blocking the Na⁺‑Cl⁻ transporter in the distal convoluted tubule. It’s less aggressive than loops, making it a good fit for mild hypertension or as an add‑on for chronic heart failure when fluid overload isn’t severe. The downside? It can raise blood sugar and may be less effective when kidney function drops below a GFR of 30 mL/min.
Bumetanide
Bumetanide is chemically similar to Furosemide but is about 40 % more potent on a milligram‑per‑milligram basis. Its rapid onset (within 30 minutes) makes it useful in hospital settings where quick diuresis is essential. Some patients who develop resistance to Furosemide respond better to bumetanide, though cost can be a limiting factor.
Torsemide
Torsemide offers a longer half‑life (about 6 hours) and more predictable bioavailability than Furosemide. It can be taken once daily for chronic management, reducing pill burden. Studies suggest torsemide may have a modest anti‑fibrotic effect on the heart, though evidence is still emerging.
Ethacrynic acid
Ethacrynic acid is the only loop diuretic that isn’t a sulfonamide, making it an option for patients allergic to sulfa drugs. It’s less commonly used because it tends to cause more ototoxicity (ear ringing or hearing loss) at high doses, and its dosing is less straightforward.
Side‑by‑Side Comparison
| Drug | Class | Onset (min) | Duration (hrs) | Typical Oral Dose | Potency (relative to Furosemide) | Cost (US, avg per tablet) |
|---|---|---|---|---|---|---|
| Furosemide | Loop | 30-60 | 6-8 | 20‑80 mg | 1× (baseline) | $0.10 |
| Hydrochlorothiazide | Thiazide | 60-120 | 12-24 | 12.5‑50 mg | ~0.2× | $0.04 |
| Bumetanide | Loop | 15-30 | 4-6 | 0.5‑2 mg | ~1.4× | $0.25 |
| Torsemide | Loop | 30-45 | 10-12 | 5‑20 mg | ~0.8× | $0.30 |
| Ethacrynic acid | Loop (non‑sulfonamide) | 30-60 | 6-8 | 50‑200 mg | ~1× | $0.45 |
When to Pick Furosemide Over the Rest
- Rapid diuresis needed: Acute pulmonary edema or pre‑operative fluid removal.
- Renal insufficiency: Loops retain potency down to a GFR of 10 mL/min, while thiazides lose effectiveness.
- Cost sensitivity: Generic Furosemide is among the cheapest prescription diuretics.
When an Alternative Might Be Smarter
- Sulfa allergy: Switch to Ethacrynic acid, despite its higher ototoxic risk.
- Long‑term outpatient control: Torsemide’s once‑daily dosing improves adherence.
- Resistance or tolerance: Bumetanide can overcome “breakthrough” fluid retention.
- Mild hypertension without edema: Hydrochlorothiazide offers blood‑pressure control with minimal fluid loss.

Safety, Side Effects, and Monitoring
All diuretics share a core set of warnings: electrolyte imbalance (especially potassium, magnesium, and sodium), dehydration, and potential kidney injury. Here’s a quick cheat‑sheet for clinicians and patients.
- Check baseline serum potassium, magnesium, and creatinine before starting.
- Re‑check labs within 3‑5 days of initiation, then weekly for the first month.
- Watch for ototoxicity-high‑dose Furosemide or rapid IV infusion can damage hearing, especially in the elderly.
- Educate patients to report dizziness, severe muscle cramps, or sudden weight gain/loss.
- Avoid concurrent NSAIDs if possible, as they blunt diuretic effect and increase kidney stress.
Practical Checklist for Choosing the Right Diuretic
- Indication: Acute edema → loop; chronic hypertension → thiazide.
- Kidney function: GFR > 30 mL/min → thiazides work; GFR < 30 mL/min → loops preferred.
- Allergy profile: Sulfa allergy → ethacrynic acid.
- Cost & insurance: Generic loop (Furosemide) is cheapest; check formulary for torsemide or bumetanide.
- Adherence concerns: Once‑daily dosing (torsemide) vs. multiple daily doses (furosemide).
- Side‑effect tolerance: If hearing issues arise, consider switching to a thiazide or lower loop dose.
Bottom Line
There’s no one‑size‑fits‑all diuretic. Furosemide remains the workhorse for fast, high‑volume fluid removal, especially when kidney function is low or cost matters. For patients needing smoother daily control, fewer pills, or who can’t tolerate sulfonamides, alternatives like torsemide, bumetanide, or ethacrynic acid fill the gaps. The key is matching the drug’s pharmacology to the clinical picture and monitoring labs closely.
Can I switch from Furosemide to a thiazide diuretic for my heart failure?
Usually not as a direct swap. Thiazides are less potent and lose effectiveness when kidney function drops, which is common in advanced heart failure. Some clinicians add a low‑dose thiazide to a loop for extra sodium loss, but they rarely replace the loop entirely.
Why does my doctor sometimes order a “potassium‑sparing” diuretic alongside Furosemide?
Loop diuretics flush large amounts of potassium. Adding a potassium‑sparing agent like spironolactone helps keep blood potassium in a safe range while still removing excess fluid.
Is torsemide really better for patients with chronic kidney disease?
Torsemide’s longer half‑life can offer steadier diuresis, and some studies suggest it may cause less rapid electrolyte swings than high‑dose furosemide. However, it’s not a cure‑all; kidney function still dictates which loop works best.
Can I take over‑the‑counter diuretics instead of a prescription?
OTC options like caffeine or herbal teas can have mild diuretic effects, but they’re unpredictable and not suitable for treating serious fluid overload. Always discuss with a healthcare provider before substituting.
What should I do if I notice ringing in my ears after starting Furosemide?
Ringing (tinnitus) can signal ototoxicity, especially with high IV doses. Contact your doctor immediately- the dose may need to be lowered or switched to another loop diuretic.
Comments (9)
-
Harry Bhullar October 21, 2025
When you start digging into the pharmacology of loop diuretics, the first thing that jumps out is just how aggressively they yank water out of the kidneys – think of it as opening the floodgates on a dam. Furosemide sits at the top of that list because it blocks the Na⁺‑K⁺‑2Cl⁻ cotransporter in the thick ascending limb, which handles roughly 15‑20 % of filtered sodium. That means you get a rapid, high‑volume urine output that’s perfect for acute scenarios like pulmonary edema or pre‑op fluid removal. The downside, of course, is the swing in electrolytes – potassium, magnesium, and sodium can all take a nosedive if you’re not careful with monitoring. Compare that to thiazides such as hydrochlorothiazide, which act further down in the distal convoluted tubule and only touch about 5‑10 % of filtered sodium; they’re milder, cheaper, and great for chronic hypertension when you don’t need a massive diuretic push. Bumetanide packs about 40 % more potency per milligram than furosemide and has a faster onset, making it a go‑to in the ICU when every minute counts, but the price tag can be a barrier for long‑term outpatient use. Torsemide, on the other hand, offers a longer half‑life and more reliable oral bioavailability, which translates into once‑daily dosing and potentially better adherence for patients who are juggling multiple pills. Ethacrynanic acid is the oddball in the group – it’s the only loop that isn’t a sulfonamide, so it’s a lifesaver for patients with sulfa allergies, yet it comes with a higher risk of ototoxicity, so you have to watch the ears closely. In practice, the choice often boils down to three pillars: the urgency of fluid removal, the patient’s renal function, and cost or insurance coverage. If you’re dealing with a GFR under 30 mL/min, loops retain efficacy where thiazides lose their punch, which is why furosemide remains the workhorse in low‑GFR settings. On the flip side, if a patient is stable, has good kidney function, and needs a maintenance regimen, torsemide’s smoother pharmacokinetic profile can reduce pill burden and provide steadier diuresis. Lastly, always pair a loop with a potassium‑sparing agent like spironolactone or a low‑dose thiazide if you need extra sodium loss without crushing potassium – it’s a balancing act that keeps patients from swinging from hyponatremia to hyperkalemia. Bottom line: understand the site of action, the onset and half‑life, and match those to the clinical scenario, and you’ll avoid a lot of trial‑and‑error while keeping side‑effects in check.
-
Dana Yonce October 31, 2025
Thanks for the clear breakdown! 😊
-
Sakib Shaikh November 11, 2025
Man, let me tell you, the moment I first saw furosemide on the med list I felt like I was staring at a superhero cape, but then the side‑effects popped up like plot twists in a drama series! The thing is, furosemide can be a bit of a wild horse – it’ll fling water out faster than a busted fire hydrant, and if you’re not watching those potassium levels, you might end up with cramps that feel like you’re doing the twist in a 90s music video. I’ve also seen patients who swear by bumetanide because it’s like furosemide’s turbo‑charged sibling, hitting the kidneys in half the time, but the price can make your wallet scream. And don’t even get me started on ethacrynic acid – the non‑sulfa hero for the allergy‑prone folks, yet it carries a sneaky risk of ringing in the ears if you crank the dose too high. Honestly, the biggest lesson is to keep labs close, because those electrolyte swings are no joke, and always have a backup plan – whether that’s a thiazide add‑on or a potassium‑sparing buddy. Bottom line: use the right tool for the job, and don’t let the “quick fix” blind you to the long‑term dance of balance.
-
Angela Koulouris November 22, 2025
Great points, and just to add a splash of color – think of the diuretics like a palette of paints. When the picture calls for a bold stroke, you reach for furosemide or bumetanide, but when you need a subtle hue, thiazides or even a potassium‑sparing agent can fill in the gaps. The key is to keep the canvas clean by monitoring labs regularly, so the artwork stays bright and not blotchy.
-
Lolita Gaela December 3, 2025
From a pharmacokinetic standpoint, the differential bioavailability of torsemide versus furosemide is a pivotal factor when optimizing outpatient regimens. Torsemide’s near‑complete oral absorption (~80‑90 %) circumvents the erratic plasma peaks seen with furosemide, which suffers from variable first‑pass metabolism. Moreover, the longer elimination half‑life (≈6 h) facilitates once‑daily dosing, thereby enhancing adherence metrics in chronic heart failure cohorts. Nevertheless, the cost–benefit analysis must incorporate formulary restrictions, as generic furosemide remains the most economical loop diuretic. In patients with sulfa hypersensitivity, ethacrynic acid serves as the non‑sulfonamide alternative, albeit with a heightened ototoxicity profile warranting audiometric surveillance. Ultimately, the therapeutic algorithm should integrate renal function thresholds, electrolyte monitoring cadence, and individual patient socioeconomic factors to tailor diuretic selection.
-
Giusto Madison December 14, 2025
Look, you can drown in all that jargon, but the bottom line is simple: if your insurance won’t cover torsemide, you’re stuck with furosemide, and you’ll have to deal with the dosing headaches. Stop whining about “pharmacokinetics” and just check labs, adjust doses, and move on. Also, don’t expect a miracle from ethacrynic acid – it’s a last‑ditch option, not a first‑line hero.
-
Kimberly Lloyd December 25, 2025
It’s fascinating how each diuretic mirrors a different philosophy of care – the aggressive loop as a bold, decisive action, while the thiazide feels like a gentle reminder to maintain balance. In the end, the patient’s lived experience is the true compass guiding our choice, reminding us that medicine is as much art as it is science.
-
Chirag Muthoo January 5, 2026
Dear colleague, I concur with the preceding reflections: the selection of diuretic therapy must be anchored in a rigorous assessment of renal function, comorbid conditions, and economic considerations. It is advisable to adhere to evidence‑based protocols and to document laboratory surveillance at stipulated intervals. Thank you for the measured discourse.
-
erica fenty January 15, 2026
Interesting summary, great insights, concise yet comprehensive, well‑written!
