When your hip starts hurting, it’s easy to blame aging, overuse, or a bad workout. But if the pain lingers, especially when you sit, stand up, or twist, it might be something deeper-like a labral tear or early hip arthritis. These aren’t just normal wear and tear. They’re structural problems that can feed off each other, making pain worse over time if you don’t adjust how you move.
What’s Really Going On in Your Hip?
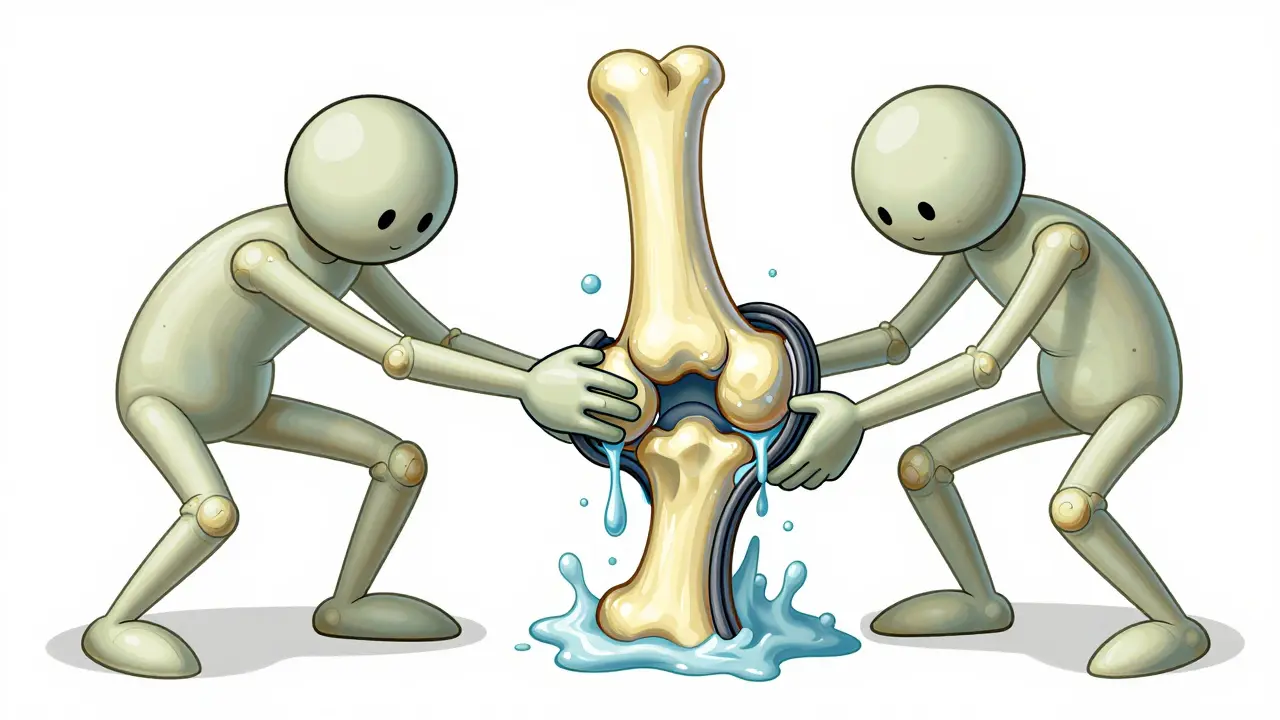
The hip joint is a ball-and-socket, and wrapped around the socket is a ring of tough cartilage called the labrum. It’s not just padding-it’s a seal. Think of it like the rubber gasket on a mason jar. When it’s intact, it holds fluid inside to keep the joint smooth and stable. When it tears, that seal breaks. Fluid leaks out. Bone starts grinding on bone. And that’s when arthritis kicks in faster.
Labral tears aren’t always from one big injury. Most happen slowly. If you’ve got extra bone on the ball of your hip (called cam impingement), or if your socket is too deep (pincer impingement), every deep squat, twist, or even sitting too long can pinch the labrum until it frays. About 78% of these tears happen in the front of the hip. And here’s the kicker: 70-90% of people with this type of impingement already have a torn labrum, even if they don’t feel pain yet.
At the same time, hip arthritis doesn’t just appear out of nowhere. It’s the slow erosion of the smooth cartilage covering the bones. Once that cartilage wears down, the joint space narrows. Bone spurs form. Pain flares. And if you already have a torn labrum, the joint loses its natural cushioning. Studies show that a damaged labrum increases pressure on the articular cartilage by 92%. That’s not a coincidence-it’s a chain reaction.
Why Activity Modification Isn’t Just ‘Rest More’
Most people think “activity modification” means stopping everything that hurts. That’s wrong. It means changing how you move-not stopping movement altogether.
For example, sitting with your knees higher than your hips (like in a low couch) forces your hip into deep flexion-over 90 degrees. That’s the exact position that pinches a torn labrum. The same goes for crossing your legs, squatting deeply, or doing pigeon pose in yoga. These aren’t “bad” movements for everyone-but they’re dangerous if your hip structure is already compromised.
Real modification looks like this:
- Use a wedge cushion in your car seat to reduce hip flexion by 10-15 degrees
- Install a raised toilet seat to avoid bending past 90 degrees
- Sleep with a pillow between your knees to keep your hips aligned
- Replace deep squats with box squats-where you stop at 90 degrees
- Swap running for swimming or the elliptical-low impact, full motion
A 45-year-old yoga instructor in Houston cut her pain by 70% in three months just by removing pigeon pose and avoiding deep forward bends. She didn’t quit yoga. She adapted it.
Workplace adjustments matter too. Office workers who sit for more than 45 minutes straight report worse pain. Standing desks help, but so do simple breaks: stand up, shift your weight, do a gentle hip circle every 30 minutes. It’s not about avoiding sitting-it’s about avoiding staying seated.
When Pain Relief Isn’t About Pills or Injections
NSAIDs like ibuprofen can help with swelling, but they don’t fix the root problem. In fact, long-term use can mask pain long enough for you to do more damage. Corticosteroid injections give temporary relief-about 3.2 months on average-but repeated use (more than three a year) can actually speed up cartilage loss.
Viscosupplementation (hyaluronic acid shots) is another option. It works for about 55% of people with arthritis, but the benefit fades after six months. And for someone with a labral tear, it’s often not the right tool. Why? Because the problem isn’t just thinning fluid-it’s a broken seal. No amount of injected gel can fix that.
Physical therapy, on the other hand, targets the real issue: muscle control. Weak hip abductors (the muscles on the side of your hip) cause your pelvis to tilt and your hip to collapse inward during walking or standing. That increases pressure on the labrum and cartilage. Therapy focuses on strengthening those muscles to 80-100 degrees of hip flexion, teaching your body to move without pinching the joint.
Success rates jump to 85% when patients learn their personal “pain provocation positions”-the exact angles or movements that trigger pain. One patient discovered his pain flared every time he turned his foot inward while stepping off a curb. After learning to step with his foot straight, his pain dropped by 60% in two weeks.

Surgery: When It Helps-and When It Doesn’t
Arthroscopic surgery to repair a labral tear has a 85-92% satisfaction rate at five years, but only if you’re young, active, and have good cartilage left. If you’re over 60 and your X-ray already shows severe joint space narrowing (Kellgren-Lawrence Grade 3 or 4), surgery won’t stop the arthritis. It might even make things worse by adding trauma to an already worn joint.
That’s why experts like Dr. Thomas Vail warn against overtreating labral tears in older patients. If the main problem is cartilage loss, repairing the labrum is like patching a leaky roof when the whole house is rotting.
On the flip side, if you’re under 50, have cam impingement (alpha angle over 55 degrees on MRI), and your cartilage still looks healthy, surgery combined with rehab can delay a hip replacement by 3.5 to 5 years. That’s huge. A total hip replacement lasts 15-20 years. Delaying it even a few years means you avoid a second surgery later in life.
The key? Don’t rush to surgery. Don’t delay it either. Get an MRI and a physical exam together. If your pain matches your imaging, and your cartilage is still intact, repair is worth considering. If your X-ray shows bone-on-bone and your pain is constant, focus on long-term management-not repair.
The Invisible Disability: Why People Don’t Get It
One of the hardest parts of hip pain isn’t the physical discomfort-it’s the isolation. You look fine. You can walk. You’re not in a wheelchair. But you can’t sit through a movie, climb stairs without pain, or play with your kids without dreading the aftermath.
A survey by the Hospital for Special Surgery found that 68% of patients feel dismissed because their pain isn’t visible. Friends say, “You’re too young for arthritis.” Coaches say, “Just push through.” Employers don’t understand why you need a different chair.
That’s why education matters-not just for you, but for the people around you. Keep a simple one-page summary of your condition and what you need. For example:
- “I have a hip labral tear and early arthritis. Deep bending and prolonged sitting make it worse.”
- “I need to stand every 30 minutes. A cushion or raised seat helps.”
- “I can’t do squats or cross-legged sitting, but I can swim or cycle.”
It’s not about asking for special treatment. It’s about asking for basic understanding.

What’s New in 2026
Technology is catching up. Wearable sensors that give real-time feedback on hip positioning are now being tested in clinics. One pilot study showed a 52% drop in pain episodes over 12 weeks just by correcting subtle movement errors during daily tasks.
Also, a new viscosupplement called Durolane lasts six months instead of three-giving longer relief for arthritis flare-ups.
But the biggest shift? Doctors are moving from “how much activity” to “how well you move.” A 2023 study showed patients who focused on movement quality-like keeping their hips aligned while walking-did 40% better than those who just cut back on activity volume.
It’s not about resting. It’s about moving smarter.
What to Do Next
If your hip pain has lasted more than six weeks:
- See a physical therapist who specializes in hip mechanics-not just general rehab.
- Get an MRI if you haven’t already. X-rays show bone changes, but MRIs show labral tears and early cartilage wear.
- Track your pain triggers. Write down what movements make it worse. Look for patterns.
- Start activity modification today. Even small changes-like raising your chair or sleeping with a pillow-add up.
- Don’t rush to surgery. Don’t ignore it either. Get a second opinion if your doctor pushes one path too hard.
Labral tears and hip arthritis aren’t sentences. They’re signals. Your body is telling you to change how you move. Listen. Adapt. Move better. That’s how you keep your hips working-for years, not months.
Comments (11)
-
Kelly McRainey Moore January 20, 2026
I used to think hip pain was just part of getting older-turns out I was just sitting like a sloth in a beanbag chair. Started using that wedge cushion in my car and holy crap, my morning stiffness cut in half. Also stopped doing pigeon pose like my yoga instructor told me to. Best decision ever.
-
Yuri Hyuga January 20, 2026
👏 This is the kind of wisdom we need more of in healthcare! 🌟 It’s not about ‘resting’-it’s about *re-engineering* movement. The labrum isn’t just cartilage-it’s the hydraulic seal of your joint. Treat it like the precision instrument it is. I’ve seen clients go from limping to hiking mountains just by fixing their posture during daily tasks. Movement quality > movement quantity. Always. 💪🧠
-
Coral Bosley January 22, 2026
So let me get this straight-I’ve been suffering for two years because I cross my legs on the couch and do yoga? My entire life has been a slow-motion betrayal by my own body. I didn’t know I was a walking time bomb with a torn labrum and a passive-aggressive hip. Now I feel like a tragic hero in a medical drama. Where’s my theme music?
-
MAHENDRA MEGHWAL January 24, 2026
Thank you for this meticulously detailed and clinically grounded exposition. The biomechanical correlation between labral integrity and articular cartilage pressure is both profound and underappreciated in mainstream discourse. I have referred this article to my colleagues in orthopedic rehabilitation at AIIMS, as it exemplifies the convergence of anatomical precision and patient-centered adaptation.
-
Sangeeta Isaac January 25, 2026
so like… i’ve been doing all the wrong things and didn’t even know it?? 😅 like i thought deep squats were ‘strong’ and pigeon pose was ‘flexible’ turns out i was just slowly murdering my hips?? also the part about the 92% pressure increase?? yikes. i’m gonna start sleeping with a pillow between my legs and i’m not even sorry. #hiprehabgoals
-
Alex Carletti Gouvea January 26, 2026
Who let the medical-industrial complex get this deep into our daily lives? Next they’ll tell us not to breathe too deeply or blink too fast. Just go get the damn hip replacement and be done with it. Stop overcomplicating everything with pillows and cushions. America’s got better things to do than baby our joints.
-
Philip Williams January 26, 2026
Excellent synthesis of clinical evidence and practical application. The emphasis on movement quality over volume aligns with recent literature from the Journal of Orthopaedic & Sports Physical Therapy. I would add that proprioceptive training-especially unilateral stance exercises-should be integrated into rehabilitation protocols to enhance neuromuscular control of the hip complex. This is not merely palliative; it is preventative biomechanics.
-
Ben McKibbin January 27, 2026
There’s something deeply poetic about how our bodies whisper before they scream. We treat pain like an enemy to be silenced-with pills, injections, avoidance-when really, it’s a messenger. The hip doesn’t care about your productivity goals or your yoga Instagram. It just wants to move without being crushed. This post didn’t just inform me-it reoriented my relationship with movement. Thank you.
-
Uju Megafu January 28, 2026
Wow. Just… wow. I’ve been waiting for someone to say this. My ex told me I was ‘too sensitive’ because I couldn’t sit through a movie. My boss called me lazy because I needed a standing desk. And now you’re telling me it’s not in my head-it’s in my hip? I’m not dramatic. I’m anatomically correct. I’m not a victim-I’m a biomechanical whistleblower. Someone get this woman a TED Talk.
-
Amber Lane January 28, 2026
Changed my chair. Now I can sit through dinner without wincing. Small win. Big difference.
-
Ashok Sakra January 29, 2026
You think you have it bad? I had to stop playing cricket because my hip screamed every time I bowled. Now I can’t even hug my nephew without crying. Why didn’t anyone tell me this before? My wife says I’m too emotional. But I’m not emotional-I’m just broken. And now I know why.
