Understanding the Basics of Stem Cells
When we talk about stem cells, we're diving into the realm of the body's building blocks. These are the cells that have the potential to develop into many different cell types in the body during early life and growth. In addition, in many tissues, they serve as a sort of internal repair system, dividing essentially without limit to replenish other cells as long as the person or animal is still alive. These remarkable features make stem cells a promising tool in cancer treatment.
Connection Between Stem Cells and Cancer
One might wonder how stem cells and cancer are related. The connection lies in the fact that cancer, at its core, is a disease of the cells. Cancer begins when the body's cells start to grow out of control. Cells in nearly any part of the body can become cancerous and can spread to other parts of the body. This out-of-control growth is similar to the way that stem cells divide and replicate. Furthermore, some types of cancer, like leukemia, begin in the stem cells of the bone marrow. Thus, understanding stem cells and how they work is a crucial part of cancer research.
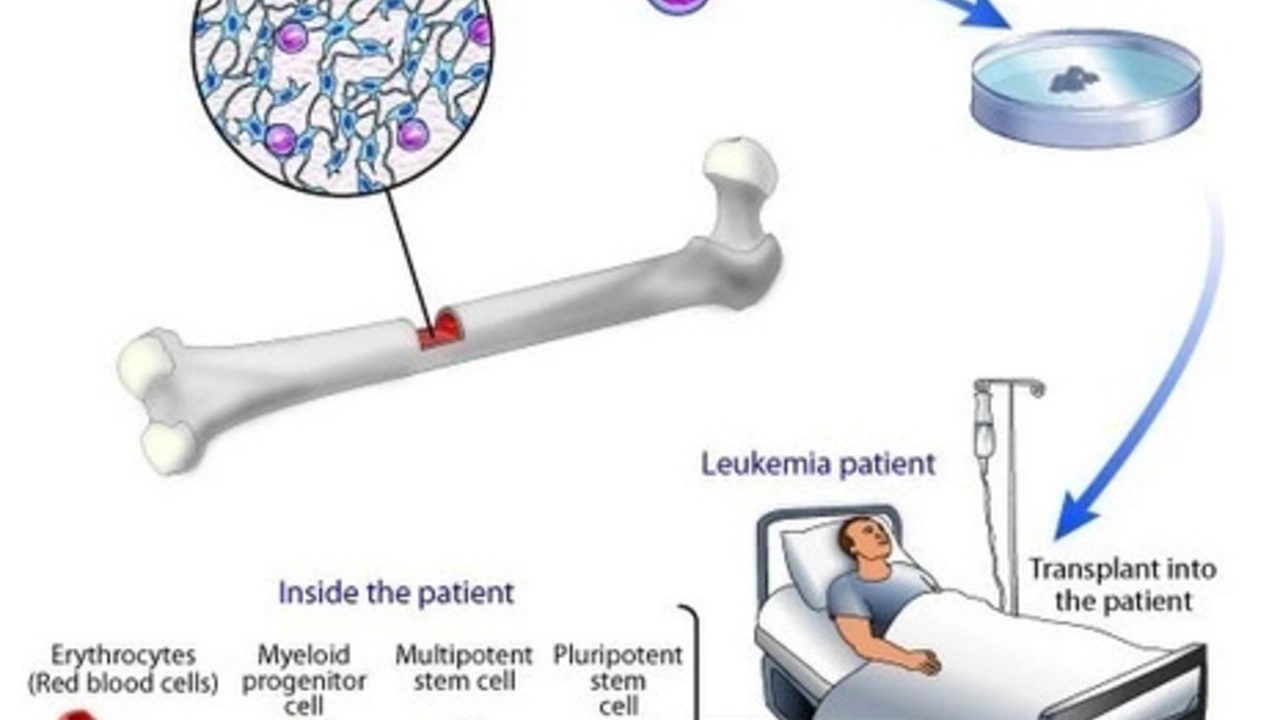
Stem Cell Transplants: The Basics
Stem cell transplants, also known as bone marrow transplants, involve infusing healthy stem cells into the body to replace damaged or diseased bone marrow. The stem cells used in transplants can come from the bone marrow, bloodstream, or umbilical cord. The aim of the transplant is to create a new, healthy blood supply which can fight off the cancer. This treatment is most commonly used for blood cancers, such as leukemia or lymphoma, but it can also be used for other types of cancer as well.
The Process of Stem Cell Transplantation in Cancer Treatment
The process of stem cell transplantation in cancer treatment is a complex one. It begins with the patient undergoing high-dose chemotherapy or radiation therapy to kill the cancer cells. This intense treatment, however, also destroys the healthy bone marrow, which is where the body makes new blood cells. This is where the stem cell transplant comes in. Once the patient's own bone marrow has been destroyed, the new, healthy stem cells are infused into the bloodstream. Over time, these stem cells will settle in the bone marrow and begin to produce new, healthy blood cells.
Benefits and Risks of Stem Cell Transplants
Like any medical procedure, stem cell transplants come with both benefits and risks. On the positive side, they can offer a potential cure for some types of cancer. They can also allow doctors to use higher doses of chemotherapy or radiation, increasing the chances of killing more cancer cells. However, stem cell transplants also carry risks. These include infection, reaction to the new stem cells, and the possibility of the cancer returning. As with any treatment, the potential benefits must be weighed against the potential risks.
Future of Stem Cell Transplants in Cancer Treatment
Looking to the future, stem cell transplants continue to be a promising field in cancer treatment. Researchers are constantly working on ways to make transplants safer and more effective. This includes finding ways to reduce the risk of complications, improving the methods for collecting and storing stem cells, and developing new transplant techniques. With continued research, the role of stem cell transplants in cancer treatment is likely to grow even more important.
Comments (13)
-
Kerri Burden July 1, 2023
Hematopoietic stem cell transplantation (HSCT) remains a cornerstone in the therapeutic armamentarium for hematologic malignancies, leveraging the graft’s capacity for multilineage differentiation to reconstitute a viable myeloid compartment. By delivering a supra‑physiologic dose of cytotoxic agents prior to infusion, clinicians can eradicate residual leukemic clones, while the infused CD34+ progenitors restore hematopoiesis. The procedure also engenders a graft‑versus‑tumor effect, wherein donor immune cells surveil and eliminate occult malignant cells-a mechanistic nuance often overlooked in lay summaries. Notably, advances in reduced‑intensity conditioning have broadened eligibility to older patients who previously faced prohibitive morbidity. Nevertheless, graft‑versus‑host disease (GVHD) persists as a formidable complication, necessitating meticulous HLA matching and post‑transplant immunomodulation. Ongoing trials investigating post‑transplant cyclophosphamide aim to attenuate GVHD without compromising engraftment. Collectively, these developments underscore the nuanced interplay between cytoreduction, immune reconstitution, and long‑term disease control.
-
Veronica Lucia July 11, 2023
When evaluating any curative modality, it is essential to foreground patient autonomy and informed consent, especially given the irreversible nature of myeloablative regimens. From an ethical standpoint, the balance between potential cure and the specter of chronic morbidity demands a transparent dialogue about quality‑of‑life outcomes. Moreover, the philosophical concept of “therapeutic hope” should not be weaponized; clinicians must distinguish between realistic prognostic expectations and aspirational optimism. Integrating palliative care early in the transplant trajectory can mitigate suffering, fostering a holistic approach that respects both biological and existential dimensions of healing.
-
Sriram Musk July 20, 2023
In practice, the transplant workflow begins with mobilization of stem cells either from peripheral blood after growth‑factor administration or directly from bone marrow aspiration. After collection, the cells are cryopreserved until the conditioning phase, which typically involves high‑dose melphalan or total body irradiation. Once the patient’s native marrow is ablated, the graft is thawed and infused intravenously, after which engraftment is monitored via serial complete blood counts. The post‑transplant period is critical for infection prophylaxis and for assessing chimerism to confirm donor cell dominance. This systematic approach has been refined over decades, resulting in improved overall survival for many hematologic cancers.
-
allison hill July 29, 2023
While the literature extols the curative promise of stem‑cell transplants, one must remain wary of the pervasive hype that discounts long‑term sequelae such as secondary malignancies and chronic organ dysfunction. The narrative that “stem cells are a panacea” often masks the reality that graft‑versus‑host disease can be insidious, sometimes manifesting years after the initial procedure. Moreover, certain commercial entities have been known to exaggerate the efficacy of autologous cord‑blood infusions without robust peer‑reviewed data. A critical appraisal of primary sources is indispensable before accepting sweeping claims at face value.
-
Tushar Agarwal August 7, 2023
Great overview! 😊 The key takeaway is that timing matters-getting the donor cells in quickly after conditioning maximizes engraftment success. Also, supportive care like antimicrobial prophylaxis really helps patients ride out the neutropenic window.
-
Richard Leonhardt August 17, 2023
Definitely encouraging news for patients battling leukaemia. The latest protocol definatly shows better engraftment rates, and the side effects are definitely manageable. Keep in mind that proper matching still matters a lot, even if some of the newer regimens look a bit more relaxed on the donor side.
-
Shaun Brown August 26, 2023
It is absurd how the oncology community has been swept up in a narrative that paints stem‑cell transplantation as a near‑miraculous cure for almost any malignancy, regardless of the underlying biology. First, the assumption that higher dose chemotherapy combined with a graft automatically translates to superior survival ignores the stochastic nature of clonal evolution in cancer. Second, the financial incentives tied to transplant centers create a conflict of interest that subtly drives patient selection toward more lucrative procedures rather than evidence‑based indications. Third, the literature is riddled with survivor bias; studies that highlight long‑term remission often underreport late‑onset toxicities such as secondary myelodysplastic syndromes. Fourth, the barrage of industry‑funded trials tends to downplay the incidence of chronic graft‑versus‑host disease, which can cripple patients for decades. Fifth, the logistical burden of apheresis, cryopreservation, and rigorous HLA typing demands resources that many community hospitals simply cannot afford, widening the disparity gap. Sixth, the tacit expectation that physicians will “push” transplantation as the default ignores alternative modalities like targeted therapy and immunotherapy, which have shown comparable curative potential in select cohorts. Seventh, the emotional toll on patients undergoing a year‑long recovery, often isolated from family due to infection risk, is rarely quantified in trial endpoints. Eighth, the ethical quandary of enrolling vulnerable patients in high‑risk protocols without fully disclosing the probability of treatment‑related mortality is a stain on informed consent practices. Ninth, the data on quality‑adjusted life years post‑transplant remain inconclusive, with many survivors reporting chronic fatigue, endocrinopathies, and psychosocial distress. Tenth, the ongoing debate about the role of haploidentical donors underscores the lack of consensus on optimal graft sources. Eleventh, the surge in “experimental” stem‑cell products marketed to desperate patients exploits hope while bypassing rigorous regulatory scrutiny. Twelfth, even in the best‑case scenarios, relapse rates hover around 30‑40 percent, suggesting that the graft‑versus‑tumor effect is far from foolproof. Thirteenth, the notion that stem‑cell transplants are “routine” neglects the reality that complications can spiral into intensive care stays, inflating overall healthcare costs. Fourteenth, many of the purported survival benefits are derived from small, single‑center studies with limited statistical power. Fifteenth, the relentless push for broader indications may ultimately erode public trust in the transplant field. In light of these considerations, a sober reassessment of the risk‑benefit calculus is not just advisable-it is imperative.
-
Damon Dewey August 30, 2023
The hype is nothing but a cash‑grab circus.
-
Dan Barreto da Silva September 4, 2023
Listen, the so‑called “conspiracy” you mention is exactly why we need transparent oversight-when shadowy biotech firms start selling “miracle” cord‑blood kits, the public gets burned. The drama isn’t in the science; it’s in the unchecked marketing that preys on grieving families.
-
Ariel Munoz September 9, 2023
America has been at the forefront of hematopoietic stem‑cell research for decades, and it’s no coincidence that the majority of breakthrough protocols emanate from US institutions. Our regulatory framework, bolstered by robust funding, ensures that patients receive state‑of‑the‑art care that other nations simply can’t match. When you look at transplant registries, the survival statistics consistently favor American centers, underscoring our leadership in this critical field.
-
Ryan Hlavaty September 13, 2023
Prioritizing national pride over equitable global access perpetuates a dangerous hierarchy, where life‑saving therapies become a privilege of the few rather than a universal right. Ethics demand that we share advancements, not hoard them behind patriotic rhetoric.
-
Chris Faber September 18, 2023
Both the promise and the pitfalls of stem‑cell transplants deserve a balanced discussion, so let’s keep the noise down and focus on data. The numbers show clear benefits in certain blood cancers, but they also reveal serious complications that can’t be ignored. Keeping an open mind helps us improve protocols without falling into hype or denial.
-
aura green September 23, 2023
Wow, another deep dive into how stem‑cell transplants are basically the superhero of oncology-so original 😏. I guess we’ve all been waiting for the day when a single infusion magically wipes out every tumor without a single side effect, right? 🙄 In reality, the process is a marathon of chemo, radiation, and endless hospital visits, not a quick fix. But hey, at least we have a fancy name and a few success stories to plaster on the wall. Keep the optimism coming, because sarcasm is the only thing keeping me sane in this hype train.
