Understanding Menopause and Vaginal Dryness
Menopause is a natural stage in a woman's life that marks the end of her reproductive years. As I entered this phase, I experienced various symptoms such as hot flashes, mood swings, and sleep disturbances. One of the most common and uncomfortable symptoms I faced was vaginal dryness, which made my intimate moments with my partner quite challenging.
Vaginal dryness occurs due to a decrease in estrogen levels, which leads to thinning and inflammation of the vaginal walls. As a result, natural lubrication is reduced, causing discomfort, itching, and pain during intercourse. In this article, I'll share some solutions that helped me find comfort during this stage of life.
1. Over-the-Counter Lubricants and Moisturizers
One of the easiest and most convenient solutions for vaginal dryness is to use over-the-counter lubricants and moisturizers. I found that water-based lubricants with no added fragrances or dyes worked best for me, as they provided instant relief during intercourse. However, it's essential to experiment with different brands and types to find the one that suits you best.
Additionally, vaginal moisturizers can be used regularly to maintain moisture in the vaginal tissues. I found that using a moisturizer every two to three days helped me manage my discomfort and maintain my overall vaginal health.
2. Natural Remedies
Being a fan of natural remedies, I decided to explore this route as well. I discovered that certain plant-based oils, such as coconut oil and vitamin E oil, can be used as natural lubricants. I also learned that consuming foods rich in phytoestrogens, such as soy products, flaxseeds, and legumes, can help balance my hormone levels and alleviate vaginal dryness.
Another natural approach I tried was incorporating regular exercise into my routine. Exercise can improve blood circulation and help maintain overall hormonal balance, which can, in turn, alleviate the symptoms of menopause, including vaginal dryness.
3. Prescription Hormone Treatments
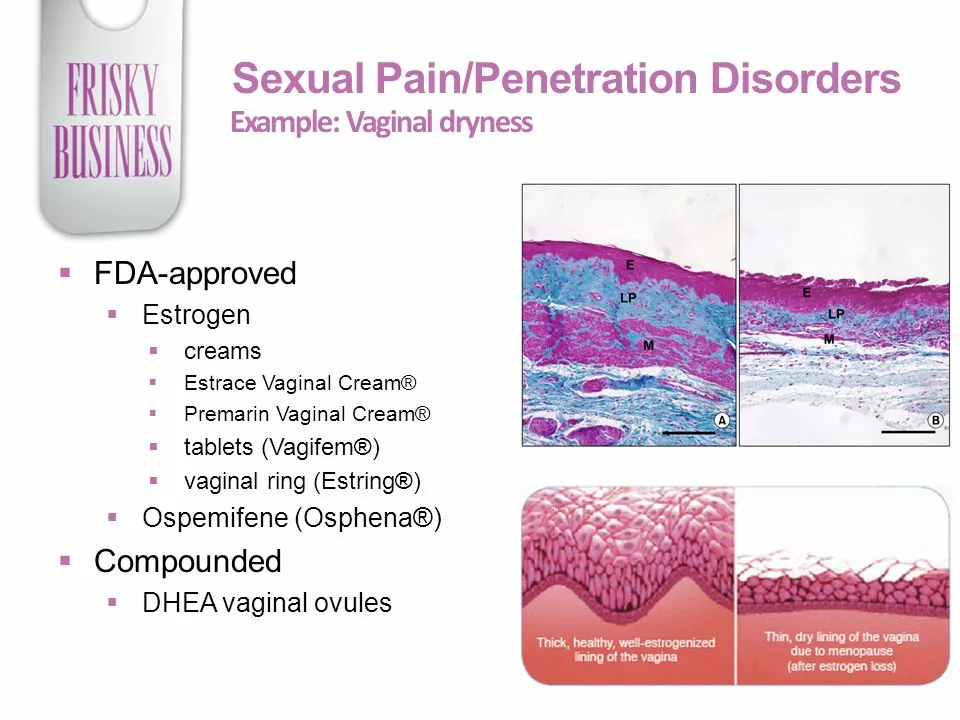
For some women, over-the-counter solutions and natural remedies may not be enough to combat vaginal dryness. In such cases, prescription hormone treatments may be an option. I consulted with my doctor, who suggested a few options, including estrogen creams, vaginal rings, and estrogen pills. These treatments can help restore estrogen levels in the body, thereby alleviating vaginal dryness and other menopausal symptoms.
It's important to discuss the potential risks and benefits of hormone treatments with a healthcare professional, as they may not be suitable for everyone.
4. Non-Hormonal Prescription Medications
If you're like me and prefer to avoid hormones, there are non-hormonal prescription medications available as well. My doctor recommended a medication called ospemifene, which helps alleviate moderate to severe vaginal dryness caused by menopause. This medication works by mimicking the effects of estrogen on the vaginal tissues without actually increasing estrogen levels in the body.
It's essential to consult with a healthcare professional before starting any prescription medication to ensure it's the right choice for you.
5. Vaginal Laser Therapy
Vaginal laser therapy is a relatively new treatment option that has gained popularity in recent years. This non-invasive procedure involves using laser energy to stimulate collagen production in the vaginal tissues, thereby increasing elasticity and moisture. I was intrigued by this treatment option and decided to give it a try. After undergoing a series of treatments, I noticed an improvement in my vaginal dryness and overall comfort.
It's important to note that vaginal laser therapy may not be suitable for everyone, and it's crucial to consult with a qualified professional to determine if it's the right choice for you.
6. Pelvic Floor Exercises
Last but not least, I discovered the benefits of pelvic floor exercises, also known as Kegel exercises. These exercises help strengthen the pelvic floor muscles, which support the uterus, bladder, and bowel. By strengthening these muscles, I was able to improve blood circulation to the vaginal area and alleviate some of the discomfort associated with vaginal dryness.
To perform Kegel exercises, simply tighten the muscles you use to stop urination, hold for a few seconds, and then relax. Repeat this process several times a day for best results.
In conclusion, menopause and vaginal dryness can be challenging to deal with, but there are various treatments and remedies available to help you find comfort. Don't be afraid to try different approaches and consult with healthcare professionals to find the best solution for you. Remember, it's essential to openly communicate with your partner about your needs and concerns during this time, as it can significantly impact your relationship and overall well-being.
Comments (14)
-
Ralph Louis April 29, 2023
Hormonal dysregulation during menopause is a textbook case of endocrine malfeasance; resorting to over‑the‑counter lubricants is a myopic band‑aid that merely masks the underlying pathophysiology. The lack of bio‑feedback integration in these products betrays a consumerist complacency that perpetuates the myth of "quick fixes". One must interrogate the pharmaco‑kinetics of estrogenic decline and recognize that superficial moisturizers do not address the vascular atrophy inherent to the vaginal epithelium. In my view, championing such products without a holistic appraisal of systemic hormonal milieu is intellectually lazy and ethically dubious.
-
Angela Allen April 29, 2023
i totally get how frustrating that can be, i went through the same thing and i found that using a gentle water based lube really helped during intimacy. also, i started a routine of using a vaginal moisturizer every few days and noticed way less irritation. the key is to listen to your body and not be afraid to try different brands until one feels right. hope this helps u feel more comfy!
-
Christopher Jimenez April 30, 2023
While the anecdotal enthusiasm for "natural oils" is pervasive, one must critically appraise the biochemistry of phytoestrogens. The literature indicates variable affinity for estrogen receptors, and the systemic impact is negligible compared to well‑studied selective estrogen receptor modulators. Moreover, the supposition that exercise alone restores mucosal hydration ignores the nuanced role of localized blood flow modulation. It would be intellectually dishonest to elevate such unsubstantiated remedies to the status of evidence‑based interventions.
-
Olivia Christensen May 1, 2023
i totally hear you 😊! while the scientific angle is important, many folks find real comfort in combining both evidence‑based treatments and gentle natural options. a balanced approach-like using a clinically approved moisturizer alongside a dash of coconut oil for added softness-can be both safe and satisfying. just remember to patch‑test any new product and keep open communication with your partner. it’s all about finding what feels best for you!
-
Lauren W May 2, 2023
Ah, the ever‑popular "just try a different brand" mantra; an approach so derivative, it borders on the banal! One would think that, after perusing the voluminous literature on estrogenic therapies, a more discerning strategy would be employed. Yet, the reticence to embrace non‑hormonal prescriptions betrays a paradoxical fear of modern pharmacology. Indeed, the over‑pursuit of conventional solutions may well eclipse the nuanced benefits of emerging modalities such as vaginal laser therapy-far too often dismissed as mere novelty.
-
Crystal Doofenschmirtz May 2, 2023
I appreciate the points raised, yet I wonder if the emphasis on laser therapy might overlook accessibility concerns for many patients. Could we perhaps explore more cost‑effective, evidence‑backed options before advocating high‑tech interventions? It would be beneficial to delineate which patient populations truly gain incremental value from such procedures. Thank you for highlighting the variety of treatments available.
-
Pankaj Kumar May 3, 2023
Hey friends, let’s keep in mind that every woman’s journey through menopause is uniquely vibrant. While some find relief in hormonal creams, others thrive with lifestyle tweaks like yoga and balanced nutrition. Encourage one another, share what’s worked, and remember that support groups can be a powerful source of comfort. You’ve got this, and we’re all here cheering you on!
-
sneha kapuri May 4, 2023
Seriously? You think slathering on some coconut oil is going to fix a complex hormonal deficiency? That’s the same pseudoscience that fuels countless “miracle cures.” Wake up and recognize that real solutions require medical supervision, not DIY kitchen experiments. Stop romanticizing ignorance.
-
Harshitha Uppada May 5, 2023
i guess we all just chill and watch the world spin while poppin a bottle of soy milk. holy moly, the whole thing sounds like a cosmic joke, dontcha think? maybe its all just a big illusion man, we are just floating in a vacuum of doubttttttttt
-
Randy Faulk May 5, 2023
Thank you for sharing such a comprehensive overview of the therapeutic options available for menopausal vaginal dryness. It is essential to begin with a thorough assessment of the patient's symptom severity, overall health status, and personal preferences. Over‑the‑counter lubricants and moisturizers provide immediate, short‑term relief and are a prudent first line for many individuals. However, clinicians should counsel patients on the importance of selecting products free from irritants such as glycerin, parabens, and artificial fragrances, as these can exacerbate discomfort.
When topical agents are insufficient, a discussion of hormone‑based therapies becomes warranted. Low‑dose vaginal estrogen preparations, such as estradiol creams, tablets, or rings, have demonstrated efficacy in restoring mucosal thickness and elasticity. These formulations deliver localized estrogen with minimal systemic absorption, thereby reducing the risk of thromboembolic events.
For patients contraindicated for estrogen, non‑hormonal prescription agents like ospemifene represent a valuable alternative. Ospemifene acts as a selective estrogen receptor modulator, improving vaginal tissue health without significantly altering systemic estrogen levels. Prior to initiating such therapy, a detailed risk‑benefit analysis should be conducted, especially in women with a history of estrogen‑sensitive malignancies.
Emerging technologies, such as fractional CO₂ laser therapy, have shown promise in enhancing collagen synthesis and vascularization within the vaginal epithelium. While preliminary data are encouraging, long‑term safety profiles remain under investigation, and insurance coverage may be limited. Patients should be counseled about the procedural nature, cost considerations, and the need for multiple treatment sessions to achieve optimal outcomes.
Adjunctive strategies, including pelvic floor rehabilitation, can augment treatment efficacy. Regular Kegel exercises improve muscular support, augmenting blood flow and potentially mitigating dryness. Lifestyle modifications, such as incorporating phytoestrogen‑rich foods, maintaining adequate hydration, and avoiding irritants like douches or scented hygiene products, further complement medical interventions.
In summary, a personalized, multimodal approach-integrating over‑the‑counter products, hormonal or non‑hormonal prescriptions, procedural options, and lifestyle modifications-offers the greatest likelihood of sustained symptom relief and enhanced quality of life. Ongoing monitoring and open patient‑provider communication remain paramount to adjust therapy as needed.
-
Brandi Hagen May 6, 2023
Wow, this thread just turned into an epic saga of menopause management! 😱 From slathering coconut oil to laser wizardry, it’s like watching a medical drama unfold. Honestly, the sheer volume of options can be overwhelming, but hey, that’s life, right? 🙄 Let’s not forget the emotional roller‑coaster-one day you’re crying over a dry night, the next you’re bragging about a new prescription that supposedly “miraculously” restores moisture. It’s a wild ride, and the drama is real! 🤦♀️
-
isabel zurutuza May 7, 2023
Sure, because a laser is exactly what I need after a bad night.
-
James Madrid May 8, 2023
Everyone’s experience is valid, and it’s great to see so many options on the table. If you’re feeling overwhelmed, consider setting a small goal-maybe try a new moisturizer for a week and track how you feel. Small steps can lead to big improvements over time.
-
Justin Valois May 8, 2023
Look, I’m not sayin we all gotta become some high end pharma plevat, but us US folks know wut’s up. The best bet is realy simple – a good old fashioned estrogen cream, nuf said. Others can keep talkin about lasern and da herbs, but if u ask me, stick to what works & has real data. No need to be a made‑up scientist.
