Understanding Central Cranial Diabetes Insipidus
Central cranial diabetes insipidus, also known as neurogenic diabetes insipidus, is a rare disorder that affects the body's ability to regulate water balance. It occurs when the pituitary gland, located at the base of the brain, fails to produce enough of a hormone called vasopressin. This hormone plays a crucial role in regulating the amount of water excreted by the kidneys. When there isn't enough vasopressin, the body loses large amounts of water through frequent urination, leading to dehydration and an increased thirst.
In this article, we will explore the connection between central cranial diabetes insipidus and vision problems, discussing the possible causes and providing practical solutions to help manage these issues.
Vision Problems Associated with Central Cranial Diabetes Insipidus
People with central cranial diabetes insipidus may experience a range of vision problems. These can include blurry or double vision, difficulty focusing, and sensitivity to light. While these issues can be uncomfortable and frustrating, it's important to remember that they are often temporary and can be managed with the right care and attention. Keep reading to learn more about the specific causes of vision problems in those with central cranial diabetes insipidus and the solutions available to help alleviate these symptoms.
Cause 1: Dehydration and Dry Eye Syndrome
One of the most common causes of vision problems in people with central cranial diabetes insipidus is dehydration. As the body loses water through frequent urination, it can lead to a decrease in tear production, resulting in dry eyes. Dry eye syndrome can cause blurry vision, discomfort, and sensitivity to light.
Fortunately, there are several treatments available to help manage dry eye syndrome. Over-the-counter artificial tears can provide temporary relief by lubricating the eyes and reducing irritation. Prescription eye drops containing cyclosporine or corticosteroids can also help to reduce inflammation and increase tear production. In more severe cases, punctal plugs can be inserted into the tear ducts to prevent tear drainage, keeping the eyes moist and comfortable.
Cause 2: Pituitary Tumors and Visual Field Defects
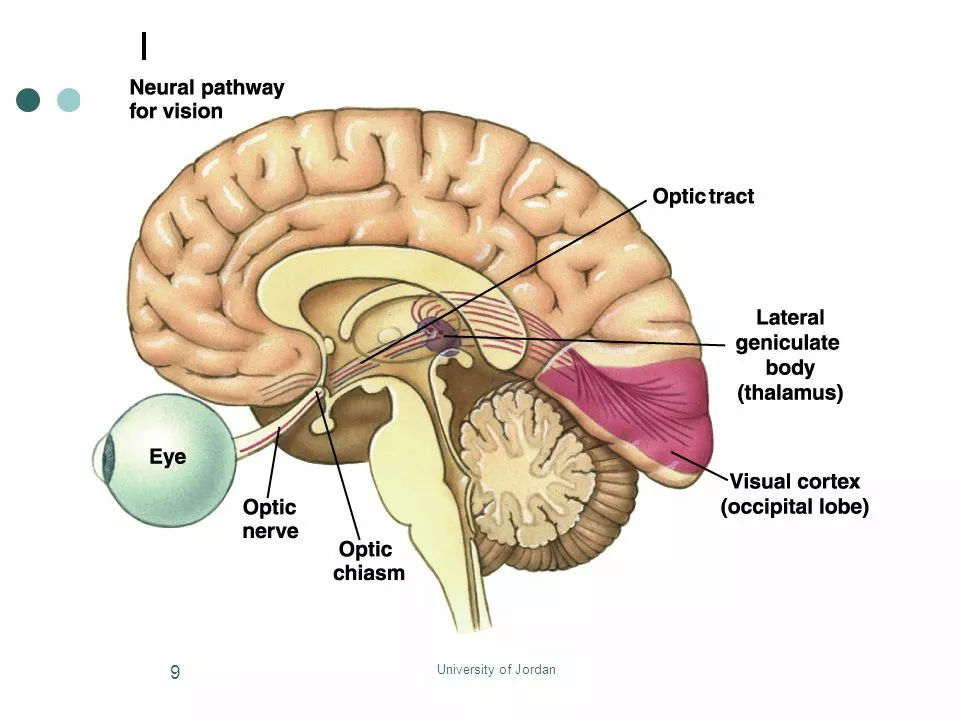
In some cases, central cranial diabetes insipidus may be caused by a pituitary tumor. When a tumor is present, it can compress the optic nerves, leading to visual field defects. These can manifest as blind spots, peripheral vision loss, or difficulty focusing on objects.
Treatment for pituitary tumors depends on the size and location of the tumor, as well as the individual's overall health. Options can include surgery, radiation therapy, or medications to shrink the tumor. Successfully treating the tumor can help to alleviate the associated vision problems.
Cause 3: Neurological Issues and Double Vision
Double vision, also known as diplopia, can be another vision problem experienced by individuals with central cranial diabetes insipidus. This can be due to neurological issues caused by the disorder or the presence of a pituitary tumor. When the nerves that control eye movement are affected, it can lead to uncoordinated eye movements and double vision.
Treatment for double vision depends on the underlying cause. In some cases, eyeglasses with prisms can help to correct the misalignment and improve vision. If a pituitary tumor is the cause, treatment options mentioned earlier, such as surgery or radiation therapy, can help to address the issue.
Managing Vision Problems: Lifestyle Changes and Self-Care
In addition to the specific treatments mentioned above, there are several lifestyle changes and self-care measures that can help to manage vision problems associated with central cranial diabetes insipidus. These include:
1. Staying well-hydrated: Drinking plenty of water throughout the day can help to prevent dehydration and alleviate dry eye symptoms.
2. Taking regular breaks from screen time: Frequent breaks from using computers, smartphones, and other devices can help to reduce eye strain and discomfort.
3. Wearing sunglasses: Protecting your eyes from bright sunlight can help to reduce light sensitivity and eye irritation.
4. Practicing good eye hygiene: Keeping the eyes clean and avoiding touching them with dirty hands can help to prevent infections and irritation.
Conclusion: Seeking Professional Help for Vision Problems
If you or a loved one has central cranial diabetes insipidus and is experiencing vision problems, it's essential to consult with a healthcare professional to determine the underlying cause and appropriate treatment options. By addressing the issue early, you can help to improve your overall quality of life and reduce the impact of vision problems on your daily activities.
Comments (17)
-
Stephen Nelson May 13, 2023
Ah, the noble art of grappling with central cranial diabetes insipidus, a topic so riveting it could make a stone weep. One might imagine the pituitary gland as a fickle poet, refusing to pen the verses of vasopressin, thereby gifting us the delightful cascade of endless urination. Of course, the accompanying vision issues are merely the universe's way of reminding us that we are not the masters of our own biology. How charming that dehydration masquerades as a fashion statement for dry eyes, while tumors play hide‑and‑seek with our optic nerves. Truly, a symphony of misery conducted by the most avant‑garde of endocrinologists.
-
Fredric Chia May 19, 2023
The exposition suffers from an overreliance on anecdotal assertions; a rigorous pharmacological analysis is requisite for substantive discourse.
-
Hope Reader May 26, 2023
Wow, thanks for the deep dive – it’s not like I’ve been Googling “dry eye syndrome” for the past hour or anything 😏. Still, the tips about staying hydrated are spot on, and I’ll definitely keep my water bottle handy while scrolling Reddit. Keep the sarcasm coming, it makes the medical jargon bearable! :)
-
Marry coral June 1, 2023
Listen up everybody, dehydration isn’t some cute side effect, it’s a nightmare that robs you of sight. You think you can just splash some water on your face and be fine? Nope, the eyes scream for relief and you’re left squinting like a bat in daylight. Get serious about drinking water, or keep living in a blurry mess!
-
Emer Kirk June 8, 2023
The cascade of symptoms begins with the relentless loss of fluid that the kidneys cannot contain and it is this unending thirst that drives the sufferer into a constant state of dehydration which then wreaks havoc upon the ocular surface reducing tear production to a near‑null level the result being a gritty, burning sensation that persists throughout the day and night the brain, deprived of adequate hydration, misfires signals that normally regulate pupil constriction leading to heightened light sensitivity and blurred vision as the cornea loses its smooth refractive properties the pituitary dysfunction can also be a harbinger of underlying neoplastic processes that compress the optic chiasm producing characteristic visual field defects the therapeutic armamentarium therefore must address both the hormonal deficit through desmopressin administration and the mechanical obstruction via surgical decompression where appropriate the role of artificial tears cannot be overstated they provide a temporary but essential mucous barrier that shields the cornea from abrasive exposure while long‑term strategies such as punctal plugs or cyclosporine eye drops sustain tear film stability the patient’s lifestyle must also adapt by scheduling regular hydration breaks limiting caffeine intake and protecting the eyes with sunglasses especially in bright environments the interdisciplinary team of endocrinologists neurologists and ophthalmologists must collaborate closely to monitor serum electrolytes visual acuity and tumor progression in order to preempt irreversible damage the journey is arduous but with diligent care the prognosis improves dramatically and the once‑blurry world regains its clarity
-
Roberta Saettone June 14, 2023
Alright, let’s cut through the haze. First, stay on top of your desmopressin schedule – missing a dose is a ticket to the desert. Second, lubricating eye drops are your new best friend; they’re cheap and effective. Third, if dry eyes persist, ask your doctor about punctal plugs – they’re small but mighty. Finally, keep an eye on any visual field changes; early detection of a tumor can save sight. And yes, that sarcasm is there because you deserve a little humor with the heavy stuff.
-
Sue Berrymore June 21, 2023
Let’s rally, folks! Dehydration isn’t just a hiccup, it’s a full‑blown call to action! Grab that water bottle like it’s a lifeline and sip before you think you need to. Remember, every glass is a victory against blurry vision. Take screen breaks, wear those stylish shades, and keep those eyes moisturized – you’ve got this! 🌟
-
Jeffrey Lee June 27, 2023
Honestly i cant beleive how many peple ignore the simple fact that staying hydrated is patriotic, our great nation thrives when its citizens are not limpidly blurrd. If you dont drink enough water you are basically givin up on american greatness. Its not rocket scince its just water, get it together.
-
Ian Parkin July 3, 2023
Dear community, I wish to extend my heartfelt encouragement to all grappling with this condition. While the challenges may seem daunting, the collective wisdom and compassionate care available are indeed a beacon of hope. May you find solace in diligent hydration and unwavering medical support.
-
Julia Odom July 10, 2023
In the grand tapestry of ocular health, one must not overlook the kaleidoscopic brilliance of proper fluid intake. I commend the earnest efforts undertaken thus far, and I implore each reader to persist with meticulous vigilance, for the eyes, like precious gemstones, demand both care and reverence.
-
Danielle Knox July 16, 2023
Well, isn’t this just another redundant pamphlet for the masses? I suppose if you enjoy reading about how to keep your eyes from drying out like a desert shrub, by all means, carry on. Might as well add a sprinkle of sarcasm for flavor.
-
Mark Evans July 23, 2023
I hear you, Danielle. Managing this condition truly feels like a marathon, but remember you’re not alone-everyone here is rooting for you. Keep taking those small steps, stay hydrated, and don’t hesitate to lean on us for support.
-
Megan C. July 29, 2023
Honestly, the only moral failing here is neglecting basic self‑care. If you can’t bother to drink water, how can you claim any higher ethical standards? The world would be better if everyone treated their bodies with the respect they deserve.
-
Greg McKinney August 5, 2023
Hydration is overrated, just drink less.
-
Dawna Rand August 11, 2023
Hey Greg, love the boldness! 🌊 Just a gentle reminder: a steady flow of water can turn that "overrated" into "essential". Keep the vibes positive! 🌟
-
Effie Chen August 18, 2023
Curious about the long‑term ocular outcomes, especially regarding optic nerve integrity. Any recent studies would be appreciated 😊.
-
rohit kulkarni August 24, 2023
In contemplating the intricate ballet of endocrine disruption and ocular dysfunction, one must first acknowledge the profound interdependence of systemic hydration and corneal homeostasis, for it is through this symbiotic relationship that the crystalline clarity of vision is either preserved or compromised, and yet, how often do we, as mere mortals, neglect the simplest of remedies-a steady influx of water-inviting, in turn, a cascade of xerophthalmic distress that besieges the delicate epithelial layers, provoking inflammation, opacity, and the dreaded sensation of sand upon the ocular surface, a sensation that, if left unchecked, may precipitate secondary complications such as keratitis or even exacerbate pre‑existing pituitary neoplasms by altering intracranial pressure, thereby further jeopardizing optic chiasm integrity; consequently, the therapeutic armamentarium must be as multifaceted as the pathology itself, encompassing not only desmopressin analogues to rectify vasopressin deficiency, but also judicious application of lubricating agents, punctal occlusion techniques, and, where indicated, surgical excision of compressive lesions, all the while fostering a patient‑centered approach that emphasizes education, compliance, and the psychosocial ramifications of chronic visual impairment, for what is a physician’s duty if not to illuminate the path toward restored sight and renewed quality of life.
